|
|
|
Indian Pediatr 2009;46: 1097-1098 |
 |
Nasopharyngeal Teratoma as a Cause
of Neonatal Stridor |
|
Lokesh Tiwari, Noopur Baijal and Jacob M Puliyel
From the Department of Pediatrics
and Neonatalogy, St Stephens Hospital, Tis Hazari,
Delhi 110 054, India.
Correspondence to:Lokesh Kumar
Tiwari, Department of Pediatrics, St Stephens
Hospital, Delhi 110054, India.
Email:
[email protected]
Received: May 14, 2008;
Initial review: June 18, 2008;
Accepted: December 29, 2008.
|
|
Abstract
We report nasopharyngeal
teratoma in a term female neonate, that presented
within first week of life with episodic stridor,
apnea and cyanosis. Laryngoscopy revealed a mass
which was confirmed by MRI. The mass was
surgically excised and diagnosed as nasopharyngeal
teratoma on histopathology. The child is doing
well on follow-up.
Keywords: Nasopharyngeal teratoma, Newborn,
Stridor.
|
|
T eratomas
are congenital neoplasia with an incidence of 1 in
40,000 live births. Teratomas in the region of the
head and
neck are relatively rare and account for less than
5% of the total(1). We report a rare case of a
congenital nasopharyngeal teratoma in a full term
neonate which presented as repeated episodes of
apnea and cyanosis. Diagnosis was delayed because
the pedunculated tumour would be lifted out of the
field of vision when the throat was examined by
direct laryngoscopy.
Case Report
A term female neonate was
transferred to neonatal intensive care unit (NICU)
at one hour of age for an episode of cyanosis and
stridor. This settled soon afterwards. On physical
examination, the facies was normal and there were no
craniofacial, maxillary or mandibular abnormalities
and no macroglossia. Initial sepsis screen, serum
glucose, calcium and electrolytes were normal. Chest
X-ray showed clear lung fields and normal
heart size.
In the NICU, the baby developed
inspiratory stridor with signs of respiratory
distress and intermittent episodes of apnea and
cyanosis, for which she was electively ventilated.
No anatomical abnormality was detected on direct
laryngoscopy. She was well on the ventilator with
minimal ventilatory settings. She was extubated
after 12 hours. On extubation the problem of
intermittent stridor recurred. Direct laryngoscopy
was repeated and this time while withdrawing the
blade of laryngoscope, a tongue like mass of about
2×1 cm was visualized hanging down from nasopharynx.
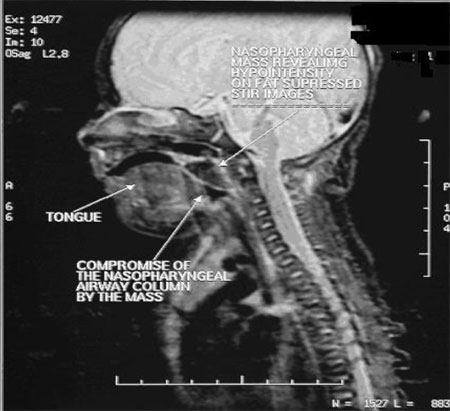
Magnetic Resonance Imaging (MRI) (Fig. 1)
confirmed a mass compromising the adjoining airway.
Surgical excision was done and histopathological
examination was consistent with mature teratoma. She
had no further episode of stridor, apnea, cyanosis
or respiratory distress and was discharged home on
day 6 of life. Child is under regular follow-up for
more than one year without any complication.
 |
|
Fig. 1 Magnetic
Resonance Scan showing a nasopharyngeal mass
compromising the adjoining airway.
|
Discussion
Generally obstructive apnea in
neonates is associated with obvious craniofacial
abnormalities including maxillary or mandibular
hypoplasia, macroglossia, or less visible
abnormalities such as laryngeal webs, laryngomalacia,
nasal polyp, nodule or other soft tissue masses.
Teratomas commonly arise from gonadal tissue and the
most frequent extra gonadal site of origin is
sacrococcygeal region(2). Teratomas in the region of
the head and neck are rare(1). There are few case
reports in the literature describing nasopharyngeal
teratoma as a cause of stridor in neonates(3,4).
Recently it has also been described in association
with other congenital malformations(5,6). In the
case reported here, the teratoma produced
intermittent life threatening obstructive apnoea. It
was difficult to diagnose because the pedunculated
tumor would be pushed up outside the field of vision
during direct laryngoscopy when the soft palate
became tense. It came into view hanging from
nasopharynx while the blade was being withdrawn and
the palate became softer.
Generally these tumors are
associated with stillbirth, perinatal death or
significant morbidity after attempted resection.
Byard, et al.(7) reported their
experience of early outcome of 18 cases (14
cervical, 4 nasopharyngeal) to demonstrate the high
morbidity and mortality that these benign but
critically placed lesions have because of their mass
effect. They usually present at or soon after birth
with signs of upper airway obstruction like stridor
or recurrent apnea. Sometimes they can be diagnosed
antenatally with the help of ultrasonography
associated with polyhydramnios. It is also
associated with increased maternal
a-fetoprotein
levels. Rarely, they may extend into the intra
cranial cavity during development. Metastasis is
rare(8).
Contributors: LT and JMP
wrote the manuscript. NB helped in author search.
Funding: None.
Competing interests: None
stated.
References
1. Shah FA, Raghuram K,
Suriyakumar G, Dave AN, Patel VB. Congenital
teratoma of nasopharynx. Indian J Radiol Imaging
2002; 12: 201-202.
2. Shetty SC, Gupta S, Cherian M,
Chary G, Shariff S. Mature teratoma of the nasal
vestibule: a case report. Ear Nose Throat J 2000;
79: 620-623.
3. de Bree R, Haasnoot K, Mahieu
HF. Teratoma in a newborn: an unusual cause of
airway obstruction. Int J Pediatr Otorhinolaryngol
1998; 44: 39-42.
4. Taweevisit M. Congenital
nasopharyngeal immature teratoma: a first case
report in Thailand. J Med Assoc Thai 2005; 88:
698-700.
5. Saha SP. Nasopharyngeal
teratoma associated with a complex congenital
cardiac anomaly. Clin Dysmorphol 2007; 16: 113-114.
6. Isken T. A congenital true
teratoma with cleft lip, palate, and columellar
sinus. J Craniofac Surg 2007; 18: 1083-1085.
7. Byard RW, Jimenez CL,
Carpenter BF, Smith CR. Congenital teratoma of the
neck and nasopharynx. A clinical and pathological
study of 18 cases. J Pediatr Child Health 1990; 26:
12-16.
8. Ülger Z, Egemen A, Karapınar
B, Veral A, Apaydin F. A very rare cause of
recurrent apnea: congenital nasopharyngeal teratoma.
Turk J Pediatr 2005; 47: 266-269.
|
|
|
 |
|

