Case Reports
Case 1: A 5 year old boy was admitted with
history of abnormal behavior, which started abruptly 3 days prior to
admission. While watching television at home, he suddenly complained that
some people were pursuing him. After this episode he was always frightened
and clung to his mother throughout the day. He became very restless,
irritable and developed violent tendencies. His speech was irrelevant and
often repetitive. He exhibited bizarre behavior like running around and
going up and down the stairs repeatedly. He refused to go to sleep and
frequently woke up crying. He refused to go to school saying that unknown
persons were pursuing him. He did not say whether he could see the people
or hear their voices.
One week prior to the onset of the symptoms he had
upper respiratory infection, which was relieved by oral medications. There
was history of recurrent otitis media up to the age of two years. The
parents did not notice any obvious hearing defect in the past. It was
reported that the child preferred right ear to listen to telephone and
sometimes gave inconsistent or irrelevant answers to questions, which the
parents attributed to carelessness.
He was an only child, born by normal delivery to
nonconsanguinous parents. His developmental milestones were normal. He was
studying in the UKG and was performing well at school. There was no family
history of mental illness.
On mental status examination he was conscious and
oriented. He was very anxious and was always clinging to his mother. His
speech was coherent but he cried frequently and answered questions after
repeated cajoling and sometimes gave irrelevant answers. His mood varied
from anxious to irritable. There were no perceptual abnormalities.
Although he had persecutory ideas they were inconsistent and their
delusional nature could not be ascertained due to his age. Since the child
was not cooperative, detailed hearing assessment could not be done. There
was no other cranial nerve involvement or focal neurological defect. Deep
tendon reflexes were normal and plantar reflex was bilaterally flexor.
His routine blood and urine examinations and CSF
analysis were normal. Brainstem auditory evoked response (BAER) evaluation
was suggestive of mild sensorineural hearing loss on the right side and
severe sensorineural hearing loss on the left side. Transient otoacoustic
emission (TOAE) test results indicated abnormal cochlear function on both
sides. MRI brain scan showed hyperintense lesions in both posterior
temperoparietal and parietal sub cortical areas on T2 and FLAIR images
which were iso- intense on T1 weighted images and were suggestive of ADEM.
He was treated with intravenous methylpre-dnisolone
30mg/kg/day for three days. Haloperidol 0.125mg twice daily for four weeks
was given to control the behavior. He improved gradually and complete
recovery occurred within a month. On follow up at six months he was using
a hearing aid on the left side and had average academic performance.
Case 2: A 10 year old girl was admitted with 3 day
history of excessive and irrelevant speech. She also complained of people
trying to attack her and her mood fluctuated rapidly. She refused to go to
school and became aggressive on minor provocations. Her sleep was
disturbed, but appetite was normal. One week prior to these symptoms she
had mild upper respiratory infection. She was born of third degree
consanguineous marriage and her developmental milestones were normal. She
was studying in the fifth standard and had good academic performance. She
was the youngest of four siblings. Her mother had psychotic illness
immediately after the second delivery, which subsided with treatment.
On examination she was conscious and oriented to time,
place and person. Her speech was coherent. Although she answered questions
relevantly, there was pressure of speech and flight of ideas. The reaction
time was shortened. Her mood was predominantly elated and occasionally
irritable. There were no definite delusions or hallucinations. Physical
examination including nervous system examination was normal.
Routine blood investigations, liver function tests, CSF
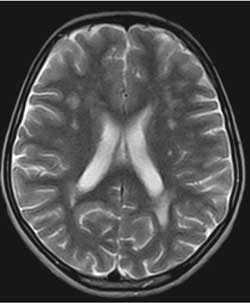
study and EEG were normal. The MRI images of brain showed focal
hyperintense areas of varying sizes in the bilateral centrum semiovale,
fronto-parietal and occipital white matter in T2 and FLAIR sequences which
were hypointense in T1 sequences (Fig.1).
 |
|
Fig. 1. MRI Image: T2 axial section
shows white matter hyperintensities. |
She was treated with intravenous methylpre-dnisolone
30mg/kg/day for three days and then switched on to oral prednisolone for
four weeks. Risperidone 0.5mg twice daily was given to control the
behavior. Her symptoms improved within two days and complete recovery
occurred after two to three weeks.
Discussion
The first child had acute onset of behavior change
characterized by excessive anxiety, restlessness, irritability,
excitement, irrelevant talk and variable mood. The persecutory delusions
were present for only brief periods. The clinical features were consistent
with a diagnosis of acute and transient psychotic disorder (F23.8) as per
the ICD-10 diagnostic criteria(6). The second child had pre-dominantly
mood symptoms. Although she had pressure of speech and flight of ideas,
the criteria for manic episode could not be satisfied. The unstable
clinical picture favored the diagnosis of acute and transient psychotic
disorder (F23.8). The MRI findings in both cases were diagnostic of ADEM.
The hearing defect in the first child was present before the illness and
hence could not be attributed to ADEM.
Psychosis is an uncommon presentation of ADEM. A
Medline database search from 1965 to 1999 identified 9 patients who
presented with acute psychosis(7). After 1999, few more cases of ADEM
presenting with psychiatric manifestations have been reported (8,9). To
the best of our knowledge, ADEM in children presenting as acute psychotic
episode has not been reported from India.
Onset of psychotic disorder during childhood is very
rare and organic causes should be ruled out in these cases. ADEM is one
possibility to be considered in such situations and MRI scan can be
helpful.
Acknowledgment
Dr PT Gaurisanker for interpretation of MRI reports.
1. Murthy JM. Acute disseminated encephalomyelitis.
Neurol India 2002; 50: 238-243.
2. Garg RK. Acute disseminated encephalomyelitis.
Postgrad Med J 2003; 79: 11-17.
3. Madan S, Aneja S, Tripathi RP, Batra A, Seth A,
Taluja V. Acute Disseminated Encephalomyelitis – A case series. Indian
Pediatr 2005; 42: 367-371.
4. Murthy SNK, Faden HS, Cohen ME, Bakshi R. Acute
disseminated encephalomyelitis in children. Pediatrics 2002; 110: e21-e21.
5. Johnston VM. Neurodegenerative disorders of
childhood. In: Kliegman RM, Behrman RE, Jenson HP, Stanton BF. Eds.
Nelson Text Book of Pediatrics. 17th Ed. Philadelphia: Saunders; 2007. p.
2499 – 2507.
6. World Health Organization. The ICD–10 Classification
of Mental and Behavioral Disorders: Clinical Descriptions and Diagnostic
Guidelines. Geneva: WHO; 1992.
7. Nasr JT, Andriola MR, Coyle PK. ADEM: Literature
review and case report of acute psychosis presentation. Pediatr Neurol
2000; 22: 8-18.
8. Lin WG, Lirng JF, Chang FC, Chen SS, Luo CB, Teng
MM, et al. Sequential MR studies of a patient with white matter
disease presenting psychotic symptoms: ADEM versus single-episode MS.
Kaohsiung J Med Sci 2001; 17: 161-166.
9. Habek M, Brinar M, Brinar VV, Poser CM. Psychiatric manifestations
of multiple sclerosis and acute disseminated encephalomyelitis. Clin
Neurol Neurosurg 2006; 108: 290-294.

