|
|
|
Indian Pediatr 2015;52: 715 |
 |
Isolated Cutaneous Cysticercosis Mimicking
Tubercular Lymphadenitis
|
|
*Birendra Rai and Farhana Sharif
Department of Pediatrics, Midland Regional Hospital, Mullingar, Westmeath, Ireland.
Email: * [email protected]
|
|
Cysticercosis is an uncommon etiology of subcutaneous
swellings in children [1]. A 6-year-old boy was referred to us as a case
of submandibular lymphadenopathy to rule out tubercular etiology. The
swelling in the left submandibular region was of 3-month duration,
insidious in onset, gradually increasing in size, and not associated
with pain or fever. There was no history of any swelling at other sites.
Examination revealed a 2◊2 cm, round, smooth non-tender swelling not
attached to the underlying muscle. General and systemic examinations
were normal. Retroviral screening was negative. Mantoux test with 1TU
was 4mm. X-Ray chest was normal. Fine needle aspiration cytology
(FNAC) revealed predominant lymphocytes and epitheloid granuloma with
caseating necrosis suggestive of tuberculosis. Since there was no
other pointers towards diagnosis of tuberculosis, we planned excisional
biopsy. Meanwhile, the cyst became tender and fluctuant requring
incision and drainage. During the procedure, along with pus, a cystic
swelling popped out that was sent for histopathological examination (Fig.
1). Biopsy revealed the presence of scolex with cyst wall
consisting of 3 layers: an outer or cuticular layer, a middle cellular
layer and an inner fibrillary layer lined by foreign body giant cells
and lymphocytes (Fig. 2). Whole body MRI and
ophthalmological examination, done to rule out disseminated
cysticercosis, were normal. The most common site of occurrence of soft
tissue cysticercosis is skeletal muscles of the upper extremities. The
viable cyst usually induces no or minimum immune response, but the dying
cysticercus (when the outer wall starts degenerating) induces
inflammation that may be associated with granuloma formation mimicking
tuberculosis.
 |
|
Fig. 1 Gross appearance of the cyst
from swelling.
|
 |
|
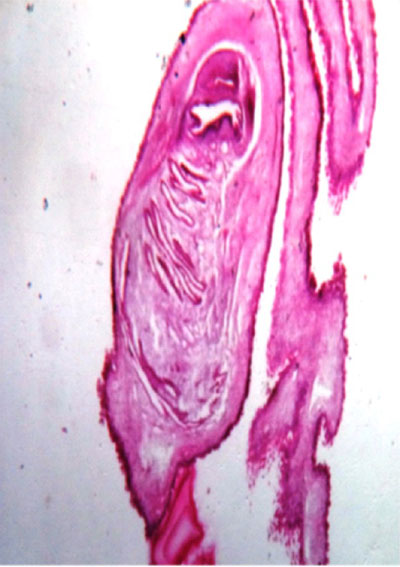
Fig. 2 Stained microsection showing
cystic wall structure. (See color image at website)
|
Cutaneous cysticerci do not carry much risk to the
patientís health, but they are often a pointer to the involvement of
internal organs, like brain [2], but also could be isolated finding [3].
Cutaneous cysts without involvement of the internal organs are treated
with excision.
References
1. Prasad KN, Prasad A, Verma A, Singh AK. Human
cysticercosis and Indian scenario: A review. J Biosci. 2008;33:571-82.
2. Arora PN, Sanchetee PC, Ramkrishan KR, Venkataram
S. Cutaneous, mucocutaneous and neurocutaneous cysticercosis. Indian J
Dermatol Venereol Leprol. 1990;56:115-8.
3. Inamadar AC, Yelikar BR. Cysticercosis cellulose cutis. Indian J
Dermatol Venereol Leprol. 2001;67:198-9.
|
|
|
 |
|

