|
|
|
Indian Pediatr 2015;52:
663-667 |
 |
Radiodensity on Serial Chest X-rays
for the Diagnosis of Foreign Body Aspiration in Children
|
|
* Eun Song Song,
*Dong Kyun Han, Hwa Jin Cho,
In Seok Jeong,
$Namsik Yoon,
Jae Sook Ma And Young
Kuk Cho
From Departments of Pediatrics and Thoracic and
Cardiovascular Surgery, Chonnam National University Hospital, Chonnam
National University Medical School;Departments of Pediatrics, Chonnam
National University Hwasun Hospital, Chonnam National University Medical
School and $The Heart Center of Chonnam National University Hospital,
the Research Institute of Medical Sciences of Chonnam National
University, Gwangju, South Korea.
Correspondence to: Young Kuk Cho, Department of
Pediatrics, Chonnam National University Medical School, 42 Jebong-ro,
Dong-gu, Gwangju 501-757, South Korea. [email protected]. *ESS and DKH
contributed equally to the paper.
Received: October 24, 2014;
Initial review: December
04, 2014;
Accepted: April 29, 2015.
|
Objectives: To evaluate the utility of measuring lung radiodensity
from chest X-ray for the diagnosis of foreign body aspiration
Methods: Records of 59 children with foreign body
aspiration were retrospectively reviewed. Lung radiodensity and
radiodensity ratio (right/left lung radio density) before and after
foreign body removal were measured. Radiodensity was calculated as the
relative score compared with the tenth thoracic vertebra body (100
points) and the background (0 point). The change of radiodensity ratio
(difference in radiodensity ratio of the second X-ray from that
of first X-ray) was compared between 22 patients (foreign body
group) and 22 normal subjects (control group).
Results: In the group of foreign body in the left
bronchus, the mean (SD) radiodensity of the left lung [53.5 (12.8)] was
lower than that of the right lung [60.8 (7.7), P<0.01] and it
increased after foreign body removal [60.0 (6.9), P=0.02]. The
radiodensity ratio decreased from 1.20 (0.30) to 0.96 (0.09) (P<0.01)
after foreign body removal. In the group with a foreign body in the
right bronchus, the radiodensity of the right lung [51.8 (12.8)] was
lower than that of left lung [62.0 (11.7), P=0.03], and it also
increased after foreign body removal [58.4 (9.6), P=0.03]. The
change of radiodensity ratio in the foreign body group [15.7 (17.8)%]
was higher than the control group [5.4 (4.3)%, P=0.01] and the
cutoff value was 7.5%.
Conclusion: Radiodensity from chest X-ray
could be a useful tool for diagnosing foreign body aspiration in
children.
Keywords: Bronchial foreign body aspiration, Chest
radiography, Diagnosis.
|
|
Foreign body aspiration is one of the most common
causes of accidental death in children under the age of 3 years [1]; the
gold standard for diagnosis is bronchoscopic inspection [2]. However,
bronchoscopy is an invasive procedure that requires general anesthesia
and may occasionally result in serious complications in children [3].
Recently, chest multidetector computed tomography (CT) was intro-duced
as a noninvasive diagnostic technique for foreign body aspiration in
children, but it has a radiation exposure hazard, in addition to reports
of false positive results [4-6].
If foreign body aspiration is suspected in adults or
well cooperating older children, patients should undergo both
inspiratory and expiratory chest X-ray [7]. However, it is
difficult to get chest X-ray at each cycle of respiration in
younger children. For them, repetitive chest X-ray can be helpful
[8].
The radiodensity of X-ray images has been used
for evaluation of physical properties of materials, such as teeth,
stone, and medications in the human body [9-11]. Unilateral emphysema or
decreased radiodensity is the typical radiological sign of foreign body
aspiration, due to the check-valve obstruction exerted by the foreign
body [8]. The purpose of this study was to evaluate the usefulness of
measuring the radiodensity from chest X-ray for the diagnosis of
foreign body aspiration.
Methods
Records of 59 patients <15 years of age who underwent
bronchoscopy through a rigid bronchoscope for the treatment of foreign
body aspiration at Chonnam National University Hospital, between January
2003 and December 2009 were retrospectively reviewed. This study was
approved by the Institutional review board of the Chonnam National
University Hospital. Among these, 22 patients (Aspiration group) had two
serial chest X-rays before bronchoscopy. Serial chest X-rays
were also collected from 22 patients without abnormal pulmonary
infiltration and respiratory symptoms (control group) from January 2003
to December 2009. Reviewed parameters included patient age, gender,
durations of symptoms before bronchoscopy, initial chest radiographic
findings, types of foreign bodies, anatomic location of foreign body,
length of hospital stay, and complications.
Radiodensity of chest X-rays: In all patients,
conventional anterior-posterior chest X-rays were performed in
the supine position using a Bucky table TH2 (Philips Medical System,
Hamburg, Germany) and read with an ADC Compact Plus storage phosphor
system (Agfa, Leverkusen, Germany). To prevent chest rotation, the chest
X-rays were rechecked when the tracheal shadow deviated from the
mediastinal area. Chest radiographic digital data were sent to a picture
archiving and communications system (PACS; Marotech, Seoul, Korea).
Photoshop CS2 imaging editing software (Adobe Systems, San Jose, CA,
USA) was used to measure the radiodensity using the histogram tool [12].
Based on different exposure to radiation, the following radio-density
scoring system was used. Lung radiodensity was determined relative to
the average radiodensity of the body of the tenth thoracic vertebra (100
points) and the background (0 points), which was outside of the body.
The margin of the lung was delimited by the rib cage, cardiac border,
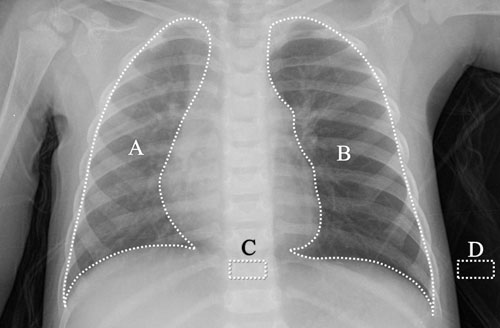
and diaphragm (Fig. 1). The lung radiodensity was
calculated as (average radiodensity of the lung [A or B] average
radiodensity of background [D]) ÷ (average radiodensity of the 10 th
thoracic vertebra body [C] average radiodensity of the background [D])
×100 (Fig. 1) [9]. The radiodensity ratio was defined as
the relative radiodensity of the right lung compared to the left lung (radiodensity
of the right lung ÷ radiodensity of the left lung). The change of
radiodensity ratio was defined as the relative change in the
radiodensity of the second X-ray from that of first X-ray
for comparison of the FBA and control groups. It was calculated (%) as
absolute value (radiodensity ratio of the first X-ray ratio of
radiodensity of the second X-ray) × 100. To evaluate
inter-observer variability in radiodensity measurements, two independent
observers blindly calculated the scoring system at different times in
the first 59 chest X-rays before foreign body removal.
Intra-observer variability analyses also were performed several months
after the primary measurements in 56 chest X-rays after foreign
body removal.
 |
|
Fig.1 Chest X-ray AP-Supine showing
the areas of radiodensity measurement.
|
Radiodensity of chest CT: Among 59 patients with
FBA, 30 (50.8%) received a chest CT using a HiSpeed Advantage helical
scanner (GE Medical Systems, Milwaukee, WI, USA) with the patient in the
supine position. CT was performed using 1-mm slice collimation from the
lung apices to the level of the adrenal glands with use of a
conventional algorithm. The scanning was performed under sedation
without a breath hold. Chest CT digital data were sent to the PACS. Lung
radiodensity by CT was calculated as average of mean value of lung
Hounsfield units (HU) on each plane.
Statistical analyses: Data are expressed as mean
(SD). The statistical analyses were performed with the Students t test
or Wilcoxon signed rank sum test, using SPSS software for Windows
version 19.0 (SPSS, Chicago, IL, USA). Receiver operator characteristic
analysis was performed to define the change of radiodensity ratio at
which the sensitivity and specificity were optimal. Correlations were
tested by using the simple linear regression method. P values
<0.05 were considered statistically significant.
Results
Table I gives the baseline characteristics of
the study subjects. The most common abnormal finding of chest X-ray
was hyperinflation (37 cases; 62.7%). Other alterations were atelectasis
(4 cases; 6.8%) and segmental atelectasis with hyperinflation (2 cases;
3.4%). The other 16 cases (27.1%) did not have definitive X-ray
abnormality. In three cases (5.1%), the foreign bodies were visible. A
chest CT was checked in 30 patients (50.8%). Among them, 21 (70%) had
definitive or suggestive foreign body, such as material in bronchus, but
the remaining 9 (30%) had no evidence of foreign body. The most common
abnormal finding from chest CT was hyperinflation (18 cases; 60%),
followed by atelectasis (5 cases; 16.7%), segmental atelectasis with
hyperinflation (3 cases; 10%), and pneumonic infiltration (2 cases;
6.7%). In contrast, two showed normal CT findings. The origin of
aspirated foreign body was predominantly vegetal (79.9% of the cases),
followed by bone (8.5%) and metallic (6.8%). There was no necessity to
perform thoracotomy. No death occurred.
TABLE I Patient Characteristics and Clinical Presentations According to the Location of the Foreign Body
|
Left bronchus (n=36) |
Right bronchus (n=14) |
Trachea or both bronchi (n=9) |
Total (n=59) |
|
Age (mo), mean (SD) |
20.5 (12.3) |
22.5 (6.7) |
22.6 (10.8) |
21.3 (10.9) |
|
Boys, n (%) |
21 (58.3) |
7 (50.0) |
6 (66.7) |
34 (57.6) |
|
Aspiration history, n (%) |
30 (83.3) |
9 (64.3) |
8 (88.9) |
47 (79.7) |
|
Lag time (d), mean (SD) |
13.5 (25.9) |
12.9 (26.2) |
2.9 (6.5) |
9.7 (21.2) |
|
Initial presentation, n (%) |
|
Cough |
28 (77.8) |
12 (85.7) |
5 (55.6) |
45 (76.3) |
|
Dyspnea |
7 (19.4) |
5 (35.7) |
4 (44.4) |
16 (27.1) |
|
Fever |
7 (19.4) |
4 (28.6) |
0 (0) |
11 (18.6) |
|
Vomiting |
4 (11.1) |
3 (21.4) |
2 (22.2) |
9 (15.3) |
|
Cyanosis |
5 (13.9) |
1 (7.14) |
2 (22.2) |
8 (13.6) |
|
Wheezing, n (%) |
13 (36.1) |
2 (14.3) |
4 (44.4) |
19 (32.2) |
|
Decreased breath sounds, n (%) |
4 (11.1) |
1 (7.1) |
0 |
5 (8.4) |
Inter-observer and intra-observer variability in the
measurement of the lung radiodensity from chest X-ray showed
excellent correlation (r = 0.96; P< 0.01 and r = 0.98; P<0.01,
respectively). The mean inter-observer and intraobserver variance were
1.2 (2.7) and 0.8 (1.5), respectively.
TABLE II Lung Radiodensity on Serial Radiographs Before and After Foreign Body Removal (N=22)
|
Location of FB |
Right lung |
Left lung |
|
Before FB removal |
After FB removal |
Before FB removal |
After FB removal |
|
Left bronchus |
60.8 (7.7) |
57.8 (8.8) |
53.5 (12.8)* |
60.0 (6.9)# |
|
Right bronchus |
51.8 (12.8) |
58.4 (9.6)* |
62.0 (11.7)* |
61.0 (9.6) |
|
Trachea both bronchi |
56.9 (7.1) |
61.9 (6.7) |
57.0 (6.4) |
64.4 (10.9) |
|
Control (n=22) |
53.9 (8.2) |
|
56.2 (8.6) |
|
|
FB: Foreign body; Data are presented as mean (SD). *P<0.05
vs right lung before FB removal. #P<0.05 vs left lung before FB
removal; Children without history of foreign body aspiration
and with normal chest X-ray. |
In those with a foreign body in either bronchus, the
radiodensity of the ipsilateral lung was lower than that of the opposite
lung (P<0.05) and it was significantly increased after foreign
body removal (Table II). Table III presents
the mean radiodensity ratio before and after foreign body removal.
TABLE III Radiodensity Ratio Before and After Foreign Body (FB) Removal
|
Location of FB |
Before removal |
After removal |
|
Left bronchus |
1.20 (0.30) |
0.96 (0.09)* |
|
Right bronchus |
0.87 (0.33) |
0.96 (0.07) |
|
Trachea or both bronchi |
1.00 (0.07) |
0.97 (0.11) |
|
FB: Foreign body; Data in mean (SD). *P<0.05 vs before FB
removal. |
The mean age of the FBA group (n=22)
undergoing serial chest X-ray was 23.6 (15.7) months and that of
the control group (n=22) was 27.3 (15.8) months. The change of
radiodensity ratio in the FBA groups [15.7 (17.8)] before foreign body
removal was significantly higher than the control groups [5.4 (4.3) %,
P=0.01], and the cutoff value in change of radiodensity ratio was
7.5% (area under the receiver operating characteristic curve
(AUC)=0.705, sensitivity 63.6%, and specificity 72.7%). Among 13 normal
findings of initial chest X-ray, 6 (46.1%) underwent serial chest
X-ray. The change of radiodensity ratio of 3 patients (50.0%)
exceeded 7.5%. After foreign body removal, the change of radiodensity
ratio in the FBA group was significantly decreased to 6.9 (4.3) % (P=0.01)
and the cutoff value in change of radiodensity ratio was 7.4%
(AUC=0.725, sensitivity 63.6%, and specificity 78.9%).
Among 35 patients with a foreign body in the left
bronchus, 15 patients (42.9%) received chest CT. The CT radiodensity of
the right lung was 609.2 (75.3) HU and that of the left lung was 655.7
(285.6) HU (P=0.08). Among 14 patients with foreign body in the
right bronchus, 9 patients (64.3%) received chest CT. The CT
radiodensity of the right lung was 723.2 (106.6) HU and that of the
left lung was 591.5 (79.8) HU (P=0.01). Among 10 patients with
foreign body in both lungs or in the trachea, 6 patients (60.0%)
received chest CT. The CT radiodensity of the right lung was 654.0
(82.6) HU and that of the left lung was 660.8 (31.3) HU (P=0.60).
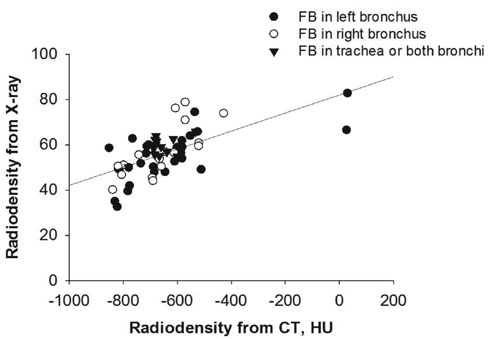
Good correlation was observed between CT radiodensity and chest X-ray
radiodensity (r = 0.64; P<0.01; Fig. 2).
 |
|
Fig. 2 Correlation between lung
radiodensity from X-ray and those from computed tomography (CT)
according to the locations of foreign body (FB).
|
Discussion
In this retrospective study, the radiodensity of the
lung ipsilateral to foreign body aspiration FBA was found to be
decreased, indicating hyperinflation caused by check valve type
obstruction, whereas the radiodensity of the contralateral lung was
increased. After removal of the foreign body, the radiodensity was
normalized in both lungs. The radiodensity ratio was normalized after
removal of the foreign body, with values similar to normal control.
We could not perform the inspiratory and expiratory
chest X-rays [14], because 93% of patients in this study were
children under the age of 3 years. Therefore, we checked serial chest
X-ray regardless of respiration and calculated the change of
radiodensity ratio. Recently, multi-detector CT was introduced as a
non-invasive technique that provides realistic 3-dimensional views of
the tracheobronchial tree [15]. We also evaluated the accuracy of chest
radiodensity compared with chest CT. In our study, the radiodensity from
X-ray showed good correlation with radiodensity from CT.
There were some limitations of this study. Among 59
patients with FBA, only 22 were checked with a repeat chest X-ray
before foreign body removal. Although all chest X-rays showed
that the trachea shadow was located in the mediastinal area, X-ray
radiodensity could be affected by body position or rotation.
In conclusion, this study indicates that the
radiodensity of the chest X-ray could be a useful tool for
diagnosing foreign body aspiration and detecting the location of the
foreign bodies in children.
Contributors: ESS, DKH, YKC: study planning,
design and writing of the manuscript; HJC, JSM: data collection and
analysis; ISJ, NY: study planning and comment. ESS and DKH contributed
equally to all aspects of this paper.
Funding: Grant (CRI 11083-31) from Chonnam
National University Hospital Biomedical Research Institute.
Competing interests: None stated.
|
What is Already Known
Conventional chest radiography has very
limited role in diagnosis of foreign body aspiration in
children.
What This Study Adds?
Radiodensity measurement in digital chest X-rays
could be a useful tool for diagnosing foreign body aspiration in
children.
|
References
1. Karakoç F, Karadağ B, Akbenlioğlu C, Ersu R,
Yildizeli B, Yüksel M, et al. Foreign body aspiration: what is
the outcome? Pediatr Pulmonol. 2002;34:30-6.
2. Adaletli I, Kurugoglu S, Ulus S, Ozer H, Elicevik
M, Kantarci F, et al. Utilization of low-dose multidetector CT
and virtual bronchoscopy in children with suspected foreign body
aspiration. Pediatr Radiol. 2007;37:33-40.
3. Zerella JT, Dimler M, McGill LC, Pippus KJ.
Foreign body aspiration in children: value of radiography and
complications of bronchoscopy. J Pediatr Surg. 1998;33: 1651-4.
4. Haliloglu M, Ciftci AO, Oto A, Gumus B, Tanyel FC,
Senocak ME, et al. CT virtual bronchoscopy in the evaluation of
children with suspected foreign body aspiration. Eur J Radiol.
2003;48:188-92.
5. Hong SJ, Goo HW, Roh JL. Utility of spiral and
cine CT scans in pediatric patients suspected of aspirating radiolucent
foreign bodies. Otolaryngol Head Neck Surg. 2008;138:576-80.
6. Koşucu P1, Ahmetoğlu A, Koramaz I, Orhan F,
Ozdemir O, Dinç H, et al. Low-dose MDCT and virtual broncho-scopy
in pediatric patients with foreign body aspiration. AJR Am J Roentgenol.
2004;183:1771-7.
7. Kim IG, Brummitt WM, Humphry A, Siomra SW, Wallace
WB. Foreign body in the airway: a review of 202 cases. Laryngoscope.
1973;83:347-54.
8. Tokar B, Ozkan R, Ilhan H. Tracheobronchial
foreign bodies in children: importance of accurate history and plain
chest radiography in delayed presentation. Clin Radiol. 2004;59:609-15.
9. Krishnamurthy MS, Ferucci PG, Sankey N, Chandhoke
PS. Is stone radiodensity a useful parameter for predicting outcome of
extracorporeal shockwave lithotripsy for stones< or = 2 cm? Int Braz J
Urol. 2005;31:3-9.
10. Fonseca R, Haiter-Neto F, Fernandes-Neto A,
Barbosa G, Soares C. Radiodensity of enamel and dentin of human, bovine
and swine teeth. Arch Oral Biol. 2004;49:919-22.
11. Florez MV, Evans JM, Daly TR. The radiodensity of
medications seen on X-ray films. Mayo Clin Proc. 1998;73:516-9.
12. Tanaka JL, Medici Filho E, Salgado JA, Salgado
MA, Moraes LC, Moraes ME, et al. Comparative analysis of human
and bovine teeth: radiographic density. Braz Oral Res. 2008;22:346-51.
13. Nah KS. The ability of panoramic radiography in
assessing maxillary sinus inflammatory diseases. Korean J Oral
Maxillofac Radiol. 2008;38:209-13.
14. Cho HK, Cho KY, Cho SY, Sohn S. Bronchial foreign
body aspiration diagnosed with MDCT. Korean J Pediatr. 2007;50:781-4.
15. Ciftci AO, Bingöl-Koloğlu M, Senocak ME, Tanyel
FC, Büyükpamukçu N. Bronchoscopy for evaluation of foreign body
aspiration in children. J Pediatr Surg. 2003;38:1170-6.
|
|
|
 |
|

