|
|
|
Indian Pediatr 2014;51:
662-663 |
 |
An Atypical Case of Parotid Gland Swelling and
Arthritis in a Child
|
|
Chandrika Azad, Adhi Arya, Vidushi Mahajan and *Shilpa
Goyal
From the Departments of Pediatrics and *Pathology,
Govt. Medical College and Hospital, Chandigarh, India.
Correspondence to: Dr Chandrika Azad, Assistant
Professor, Department of Pediatrics, Govt. Medical College and Hospital,
Sector 32, Chandigarh 160 030, India.
Email:
[email protected]
Received: February 18, 2014;
Initial review: April 09, 2014;
Accepted: May 30, 2014.
|
|
Background: Early onset
sarcoidosis is a rarely reported disease in children. Case
characteristics: 2½-year-old girl with chronic enlargement of
bilateral parotid glands and polyarthritis. Observation: Biopsy
of salivary gland revealed non-caseating granuloma. Outcome:
Polyarthritis and salivary gland swelling resolved completely after
starting oral corticosteroids. Message: Sarcoidosis is an
important differential diagnosis in young children with joint and
salivary gland involvement.
Keywords: Arthritis, Parotitis, Sarcoidosis.
|
|
S
arcoidosis in pediatric age group is rare with an
incidence of 0.22-0.27 per 100,000 children per year; incidence is 0.06
in children ≤4
years of age and increases gradually to 1.02 in children aged 14-15
years [1]. Only few cases have been reported from India [2]. It can be
difficult to diagnose because of its rarity and similarity to other
common disorders like tuberculosis and juvenile idiopathic arthritis
(JIA). We hereby report a young child with arthritis and salivary gland
involvement.
Case Report
A 2½-year-old girl, resident of Hilly area of
Northern India, presented with joint swellings for two years, and
swelling in pre-auricular area and fever for two months. The joint
swellings were painless (painful only during winter season) and boggy,
involving ankles, knees and wrist joints, with some relief on oral
medications but it never resolved completely. There was no history of
rash, cough, dryness of mouth or eyes, weight loss, con-vulsions, or
previous hospital admissions. Family history was non-contributory; there
was no history of tuberculosis. On examination, child had stable vitals,
with weight <3rd percentile and height between 3rd and 15th percentile.
There was generalized non-tender and non-matted lymphadenopathy along
with mild pallor. Submandibular and parotid glands were enlarged (Fig.
1), non-tender and soft to firm in consistency. There was no
icterus, cyanosis, edema or clubbing. Soft, fluctuant and non-tender
swelling was present bilaterally above knees, ankles and wrist joints.
There was no corneal or conjunctival dryness or uveitis. Systemic
examination was non-contributory. Provisional diagnosis of systemic
onset JIA was kept.
 |
|
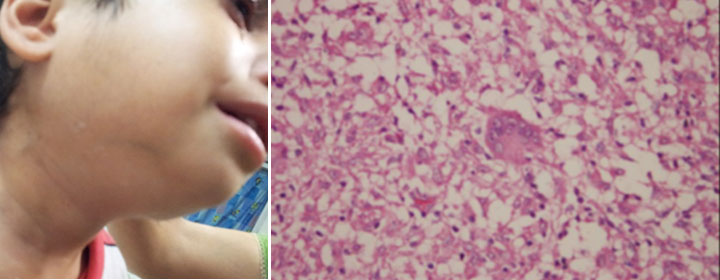
Fig. 1 (a) Enlarged parotid and
submandibular salivary glands; (b) Histology from submandibular
gland showing non-caseating granuloma with langhans giant cell.
|
Hematological workup was normal except microcytic,
hypochromic anemia and raised erythrocyte sedimentation rate. Serum
electrolytes and renal function tests were within normal limits. Serum
Angiotensin Converting Enzyme (SACE) was 190 U/L (Normal 8-52 IU/L) and
Urinary calcium was normal (0.12 g/L). Serum immunoglobulins, calcium,
phos-phorus, alkaline phosphatase and uric acid were within normal
limits. Antinuclear Antibody, RA factor and Antistreptolysin-O titers
were not raised. C-reactive protein was increased. HIV and tubercular
workup were negative. Ultrasonography (USG) of knee joint showed
suppurative fluid collection over both patellar bursae. X-ray of
the joints did not show any erosion. USG abdomen showed increased renal
echogenicity and minimal bowel fluid. Fine needle aspiration cytology
(FNAC) of knee joint showed synovial hyperplasia, and FNAC of right
parotid and left submandibular area showed non-caseating granuloma.
Biopsy from the submandibular gland also showed non-caseating granulomas
with no acid-fast bacilli. Final diagnosis of sarcoidosis was made and
the child was started on prednisolone (2mg/kg/day). Within two weeks,
submandibular and parotid swelling subsided completely. In next two
weeks, her joint swelling also subsided. Steroids were given on
alternate days after four weeks, and then gradually tapered to 0.5
mg/kg/d every alternate day. She is completely asymptomatic after one
year of follow-up.
Discussion
Sarcoidosis is a rare multisystem disorder, affecting
most of the organ systems. In younger children, diagnosis is often
challenging as presentation is very different from that seen in older
children and adults [1]. Young children (<5 years of age) present with
classical triad of rash, polyarthritis and uveitis [3]; our patient did
not present with this triad. Arthritis of sarcoidosis is characterized
by painless boggy effusions of synovium without limitation of motion
[4], as seen in our patient. The seasonal variation of arthritis, as
seen in our child, has been reported earlier [5].
A close differential diagnosis in the index case was
Blau syndrome, which classically presents as granulo-matous dermatitis,
arthritis and uveitis; salivary gland involvement may also occur.
Although clinical features in our patient were suggestive of Blau
syndrome, there was no family history of similar illness and no joint
erosion on X-ray as seen in blau syndrome [6]. Some authors
consider Blau syndrome and early onset sarcoidosis to be familial and
sporadic forms of the same disease [7,8]. We could not get mutation
analysis for CARD15/NOD2. Another important differential was
systemic-onset JIA but non-erosive boggy arthritis favoured sarcoidosis.
Granulomatous salivary gland involvement – as seen in our patient – can
be found in a variety of disorders, including infections, autoimmune
disorders and sarcoidosis [9]. In sarcoidosis, parotid involvement is
seen in 6% of adult cases and is commoner in females [10]. In a case
series from India, one out of 12 patients had parotid involvement, and
eight patients presented with arthritis [2].
There is no gold standard diagnostic test for
sarcoidosis. Although SACE can be increased in more than half of
children with late-onset sarcoidosis, it is not specific for sarcoidosis.
Usually the diagnosis is made by demonstrating a typical non-caseating
epithelioid cell granuloma on a biopsy specimen that can also be seen in
tuberculosis, leprosy, Sjogren syndrome, Behcet disease and berylliosis
[1,3].
Prognosis in sarcoidosis of early onset is guarded;
there is likelihood of chronic progressive course and sequelae in large
proportion of patients [3]. We conclude that possibility of sarcoidosis
should always be kept in any child presenting with chronic arthritis or
salivary gland involvement.
References
1. Hoffmann AL, Milman N, Byg KE. Childhood
sarcoidosis in Denmark 1979-1994: Incidence, clinical features and
laboratory results at presentation in 48 children. Acta Paediatr.
2004;93:30-6.
2. Gupta SK. Pediatric sarcoidosis in India. Indian J
Pediatr. 2001;68:931-5.
3. Häfner R, Vogel P. Sarcoidosis of early onset: A
challenge for the pediatric rheumatologist. Clin Exp Rheumatol. 1993;11:
685-91.
4. Rosenberg AM, Yee EH, MacKenzie JW. Arthritis in
childhood sarcoidosis. J Rheumatol. 1983;10:987-90.
5. Glennas A, Kvien TK, Melby K, Refvem OK, Andrup O,
Karstensen B, et al. Acute sarcoid arthritis: Occurrence,
seasonal onset, clinical features and outcome. Br J Rheumatol.
1995;34:45-50.
6. Sfriso P, Caso F, Tognon S, Galozzi P, Gava A,
Punzi L. Blau syndrome: clinical and genetic aspects. Auto-immunity
Reviews. 2012;12:44-51.
7. Kanazawa N, Okafuji I, Kambe N, Nishikomori R,
Nakata-Hizume M, Nagai S, et al. Early-onset sarcoidosis and
CARD15 mutations with constitutive nuclear factor-kappa B activation:
common genetic etiology with Blau syndrome. Blood. 2005;105:1195-7.
8. Rose CD, Doyle TM, McIlvain-Simpson G, Coffman JE,
Rosenbaum JT, Davey MP, et al. Blau syndrome mutation of
CARD15/NOD2 in sporadic early onset granulomatous arthritis. J Rheumatol.
2005;32:373-5.
9. Vanhauwaert BG, Roskams TA, Vanneste SB, Knockaert
DC. Salivary gland involvement as initial presentation of Wegener’s
disease. Postgrad Med J. 1993; 69, 643-5.
10. James DG, Sharma OP. Parotid gland sarcoidosis. Sarcoidosis Vasc
Diffuse Lung Dis. 2000;17:27-32.
|
|
|
 |
|

