|
D
evelopment is a continuous process that occurs
normally in childhood, wherein skills are acquired in various
inter-related developmental domains. It is intricately influenced by a
combination of genetic, biological and psycho-social factors [1].
Pediatricians frequently face parental concerns regarding development
and/or behavior [2]. Some of these issues may be transient and easily
rectifiable but a small but significant proportion may actually be
harbingers of neuro-developmental disorders.
The global prevalence of developmental delay in
children is reported as 1-3%, while World Health Organization (WHO)
estimates that 15% of the world’s population lives with some form of
disability [3,4]. There is a paucity of community-based data from lower
and middle income countries (LMIC), but a similar or higher prevalence
is expected [5]. Due to improving maternal and child health care and
better neonatal and child survival, there is now a large group of
children at high risk for developmental delay in these countries. In
addition, the proportion of children experiencing poverty, ill-health,
malnutrition and lack of early stimulation – factors that adversely
affect attaining optimum developmental potential – are much more in
comparison to high income countries [1].
One of the main reasons for lack of community-based
data from India is the absence of routine developmental screening and
surveillance. Developmental surveillance is the longitudinal process of
identification and monitoring of newborns and children at high risk [6].
This comprises of eliciting parental concerns, acquiring developmental
history, identifying risk and protective factors, evaluation, and
maintenance of records [7]. Screening is the brief cross-sectional
process of evaluating children by screening tools with good psychometric
qualities (sensitivity and specificity >70-80%), that have been
norm-referenced and standardized on populations representative of the
target population [5-7]. In developed countries, both strategies are
core components of the health, education and social care systems [8].
The American Academy of Pediatrics (AAP) recommends developmental
surveillance of high-risk children at each health visit from birth to 3
years, and routine screening of low-risk children at 9, 18, and 24/30
months or earlier if concerns are elicited [7]. Screening for behavioral
disorders and academic/learning disorders is also recommended [9]. Hix-Small,
et al. [10] reported an increase in screening in USA after these
guidelines were framed, though it is still far from ideal. Lack of
screening means delay in detection, initiation of intervention,
increased morbidity and parental anguish, more health service
utilization and poorer prognosis [11].
Why Developmental Screening is not Routinely Practiced in India?
In India, there are multiple challenges to practice
of universal developmental surveillance and screening. Parents are
unaware of the existence and need of these services. Health care seeking
is prioritized for acute illnesses which are not appropriate
opportunities for screening. A heterogeneous population of doctors with
variable proficiency caters to the health needs of Indian children. If
parents express concerns, they are often given false assurances without
proper appraisal. Well-child visits are primarily for immunization with
a few perfunctory questions asked about development, if at all. This was
documented in a study of perceptions and practices of 90 pediatricians
from Gujrat [12]. Most participants (97.3%) reported parents expressing
developmental concerns but only 13.6% used structured tools for
evaluation. Reasons cited by those relying on informal assessment were
time constraints (72%), non-availability of treatment or referral
options (45%), and inability to use screening tools (28%). Contrary to
this common misconception, informal evaluation has been proved
unreliable in detecting developmental delay. Recognition is difficult in
early childhood unless specifically looked for in a structured way,
since changes in development are rapid, there is intra-domain overlap,
and early indicators are often subtle.
At present, exposure and training in formal
developmental screening and assessment is lacking in the post-graduate
pediatric curriculum. Pediatricians may be cognitively aware but lack
the necessary psycho-motor and communication skills to screen
effectively. There is a scarcity of developmental pediatricians.
Available assessment tools are mostly of international origin, which are
expensive, not easily available, and require training and accreditation.
Recommendations for developmental screening by the Indian Academy of
Pediatrics (IAP) are yet to be formulated. Although the ‘Persons with
Disabilities Act, 1995’ states that ‘children should be screened
annually to detect high risk cases’, the process is not outlined [13].
In 2013, the ‘Rashtriya Bal Swasthya Karyakram (RBSK)’ was
launched by the Government of India, which aims at screening for defects
at birth, diseases, deficiencies and development delays including
disabilities (4 D’s) in children between 0 to 18 years [14]. It is
envisioned that pre-school children will be screened by Anganwadi
workers using age-appropriate developmental checklists in the periphery
and the positive cases will be re-assessed by trained personnel at the
secondary and tertiary care levels. Once this swings into action there
will naturally be an upsurge of pediatric consultations by concerned
parents, which will need to be tackled responsibly. Reviews of screening
tools that may be used in LMICs are available but are hampered by lack
of clear guidelines or practice algorithms [5,15,16].
This article aims at sensitizing pediatricians,
reviewing certain general (not domain-specific) developmental screening
and monitoring tools validated for use in Indian under-five children,
and proposes an office practice paradigm.
Developmental Screening Tools in Use in India
Screening tools currently in use in India include
those developed and validated in high-income countries, translations of
the above in Indian languages, and indigenously developed tools. Each
type has its own problems. In addition to the drawbacks outlined
earlier, internationally acclaimed tools may not be suitable for our
populations due to presence of items that are culturally alien or which
lose context after translation. They also require validation on large
reference groups comprising of healthy children of the target population
without conditions averse to development like iron deficiency anemia,
malnutrition, poverty, and decreased stimulation [17]. Translations may
be understandable but still face the aforementioned drawbacks, unless
validated. Indian tools are language and culturally suitable, have been
validated but may not have optimal psychometric properties since most
were originally developed largely for community surveys by health
workers. Taking these aspects into consideration, a list of screening
tools for developmental delay popularly in use or validated in Indian
settings was compiled and those that could be administered by
pediatricians in any office setting were reviewed. Tools screening for
behavior problems or specific domains or overt disability were not
included.
Analytically Comparing Tools for Development Screening
To be able to compare tools qualitatively, it is
essential to understand their characteristics. Table I
outlines the definitions and acceptable standards of commonly used
psychometric parameters. These are important for making educated
decisions regarding quality. If screening tools are not used for their
intended purpose (i.e. screening tools being used for diagnosis
or in children outside the intended age range), reliability gets
compromised. Choice of tools also differs according to level of risk for
developmental delay; high-risk children being those with biological
and/or environmental risk factors. Constituent items of tools may be
historically based (milestones, opportunity-based skills),
performance-based or both. In contrast to developed counties, parental
interviews are not as reliable in LMICs due to poorer literacy levels,
unawareness of milestones and possibility of socially acceptable
responses being given due to associated social stigma [5,15,16].
Interpretation of a screening result as pass or fail is done by
comparing with scores derived from standardized population
norm-references or pre-decided performance criterion.
TABLE I Definitions and Acceptable Standards of Development Tool Related Psychometric Properties
|
Term |
Description |
Acceptable standard |
|
Standardization |
The uniformity of procedure in administering and scoring the
test
|
On representative
|
|
exactly as outlined by the developer of the tool.
|
population |
|
Validity |
The ability of a tool to assess what it is intended to assess in
|
70% |
|
comparison with a gold standard diagnostic tool |
|
|
Sensitivity |
Percentage of children with delay/ problem who are correctly
|
70 80% |
|
identified by the screening test
|
|
|
Specificity
|
Percentage of children without delay/ problem who are correctly |
³80%
|
|
identified by the screening test
|
|
|
Positive Predictive Value
|
Percentage of children identified with delay/ problem by the
|
30-50% |
|
screening test who do indeed have the delay/ problem |
|
|
Negative Predictive Value
|
Percentage of children identified as normally developing by the
|
|
|
screening test who are indeed developing normally |
|
|
Reliability |
How consistently similar results are obtained repeatedly |
High/ strong-
|
|
Inter-rater |
Result variability if test given by different interviewers |
coefficients>0.60 |
|
Test-retest
|
Result variability when repeated later
|
|
Deciding the Tool Best Suited for Indian Children
Hypothetically, an ideal screening tool for Indian
children is a brief, inexpensive tool with good psychometric properties,
available in Indian languages, comprising of purely
developmental/culturally-adapted items, that has been validated on
representative healthy Indian children and requiring minimal training
[17]. Such a designer tool does not exist in reality; so each
pediatrician has to make an educated choice best suited for individual
practice. Developmental tools of international origin are compared in
Table II. Only two of these have been validated in Indian
children.
TABLE II Comparison of Developmental Screening Tools of International Origin
|
Factors |
Denver DevelopmentalScreening Test II |
Bayley Infant Neuro-developmental Screen (BINS) |
Parents Evaluationof Developmental Status (PEDS)
|
Ages and stages questionnaire (ASQ)
|
Developmental* Profile II/ III
|
|
Age Format |
0-6 yearsDirectly administered |
3-24 monthDirectly administered
|
0-8 yearsParent-report |
1 -66 /3- 66 mParent report |
0-9 y/ 12 y11m Parent report
|
|
Screens/Domains |
Expressive & receptivelanguage, gross motor, fine motor,
personalsocial
|
Neurological processes, expressive and receptive functions&
cognitive |
Cognitive, expressive& receptive language fine &
gross motor, social-emotional, behavior, self-help& school |
Communication, gross motor, fine motor,problem-solving,
andpersonal adaptive skills |
Physical, Self-help/ Adaptive, Social/Social-emotional,Academic/
cognitiveand Communication
|
|
Itemsont> |
125 |
11-13 |
10
|
22-36 |
186/ 180 |
|
Scoring/ Result |
Risk category: normal/abnormal/ questionable |
Risk category: high/ low moderate |
Risk category: low/ medium/ high |
Pass/fail scores |
Total score gives domain wise age equivalents |
|
Time
|
10-20 min
|
10 min |
2-10 min |
10-15 min |
10 /20-40 min |
|
Language |
English, Spanish |
English |
English |
English, Hindi |
English |
|
Psychometric
|
Sensitivity 0.56-0.83 |
Sensitivity 0.75-0.86 |
Sensitivity 0.74-0.79 |
Sensitivity 0.70-0.90 |
Validity Coefficients*
|
|
properties |
Specificity 0.43-0.80
|
Specificity 0.75-0.86 |
Specificity 0.70-0.80 |
Specificity 0.76-0.91
|
0.52-0.72
|
|
Validated in India |
Not validated |
Not validated |
Sensitivity 62% Specificity 65% |
Sensitivity 83.3% Specificity 75.4% |
Not validated but used extensively |
|
Cost
|
$111
|
$325
|
$30
|
$249 |
$240
|
|
Access site |
http://www.denverii.com/ |
www.pearsonassessments.com
|
www.pedstest.com
|
www.brookespub lishing.com/asq |
www.wpspublish.com
|
|
*Internal consistency: 0.89-0.97 and Test-retest reliability:
0.81-0.92
|
The Denver Developmental Screening Test (DDST) is a
very popular and frequently used international screening test [18-20].
However, its low specificity (43%) leads to over identification of false
positives, parental apprehension, and burden on the system for diagnosis
and intervention. Hence it is no longer considered appropriate for the
purpose of screening. The Bayley Infant Neuro-developmental Screen
(BINS) has been used for monitoring children at moderate to severe high
risk [21,22]. Though psychometric properties are acceptable, its
drawbacks are lack of validation in Indian children and inability to
screen children beyond 2 years of age. The Ages and Stages Questionnaire
(ASQ) is a parent- completed questionnaire with acceptable properties
[23]. In a study by Juneja, et al. [24], ASQ was validated
against the Developmental Scale for Assessment of Indian Infants. After
being translated into Hindi and substitution of a few culturally
inappropriate items, this version of ASQ was administered to parents by
an interviewer to screen children aged 4,10,18 and 24 months with both
high and low risk. The overall sensitivity in detecting developmental
delay was 83.3% (higher for the high-risk children), specificity 75.4%
and negative predictive value 84.6%. ASQ has the potential to be used in
India after being translated into local languages if interviewer-
administration replaces parent-completion when required.
Studies in the West have shown that asking parents
about development concerns is reliable for assessment [25]. Parent
Evaluation of Developmental Status (PEDS) considers concerns as either
‘not predictive’ or ‘predictive’ of developmental disabilities. The
latter categorizes children as having High, Moderate or Low risk of
developmental disabilities. Each is linked with related management
protocols: referral, more screening or continued surveillance,
respectively. PEDS has been found reliable in other developing
countries; however, there is limited literature from India [19,26,27].
The only available study from India was by Malhi, et al. [28] in
which it was compared with Developmental Profile II (DP II) and Vineland
Social Maturity Scale. Psychometric properties were found to be
sub-optimal. The authors suggested that PEDS could be used to identify
children requiring in-depth screening in situations involving time
constraints. The limitations of this study were use of another screening
tool as gold standard and a small sample size. Further research is
warranted before its value in the Indian context is clarified [5,15].
Developmental Profile III is an updated version of DP II that screens
for developmental delay in five key areas [29,30]. Its norms are based
on a large representative sample of typically developing American
children. Although used in India frequently in numerous research
studies, it is yet to be validated in Indian children.
Indian screening tools, that were designed for
community surveys but can be used for office practice, are compared in
Table III. These are easy to perform and interpret,
inexpensive, and have been norm-referenced and standardized in
representative populations. The main drawback is less than acceptable
psychometric properties. Normative data of both Baroda Developmental
Screening Test (BDST) and Trivandrum Developmental Screening Chart
(TDSC) are derived from the Bayley Scales of Infant Development (BSID)
which has not been re-validated since its inception more than 20 years
ago [31]. The same drawback lies in the Indian Council Medical Research
Psychosocial Developmental Screening Test (ICMR-PDST) [32,33]. In the
TDSC validation study, the gold standard that was used was not a
diagnostic tool but DDST (no longer considered suitable): so the results
may be considered questionable until re-validated against a more robust
gold standard [34].
TABLE III Comparison of Indian Developmental Screening Tools
|
Factors |
Baroda Developmental
|
Trivandrum Developmental
|
ICMR Psychosocial developmental
|
|
screening Test (BDST) |
Screening Chart (TDSC) [25] |
screening Test [27, 28] |
|
[24] |
|
|
|
Developed from |
Bayley Scales of Infant
|
Bayley Scales of Infant
|
Programme for Estimating Age-related
|
|
Development, Normative data |
Development (Baroda Norms)
|
Centiles Using Piece-wise Polynomials*
|
|
from Indian children |
|
Normative data from Indian children |
|
Age |
0 - 30 mo |
0 - 24 mo |
0-6 y
|
|
Format |
Directly administered |
Directly administered
|
Parent interview 66 items
|
|
54 items
|
17 items |
|
|
Domains |
Motor and Cognitive
|
Mental and Motor
|
Gross Motor, Vision & Fine motor,
|
|
|
|
Hearing, language & concept development,
|
|
|
|
Self Help & Social skills |
|
Scoring/ Result
|
Age equivalent and |
Within age range |
3rd, 5th, 25th, 50th, 75th, 95th & 97th
|
|
developmental
|
|
centiles given Significant delay < 3rd centile
|
|
quotient calculated |
|
(2 S.D) |
|
Training |
Minimal training
|
Minimal training |
None |
|
Setting
|
Community/ office
|
Community/ office
|
Community/ office
|
|
Time taken |
10 min
|
5 min |
Minimal
|
|
Psychometric
|
Sensitivity: 65-93%,
|
Sensitivity: 66.8%,
|
Not given |
|
properties
|
Specificity: 77.4-94.4% |
Specificity: 78.8% |
|
|
PPV: 6.67-34.37% |
|
|
|
Access site &
|
Promila Phatak,
|
MKC Nair, Child |
ICMR, Free
|
|
Cost
|
Department of Child
|
Developmental Centre
|
|
|
Development, University
|
Trivandrum, Kerala, India. |
|
|
of Baroda, India.
|
Inexpensive |
|
|
Inexpensive |
|
|
|
ICMR: Indian Council of Medical Research, PPV: Positive
Predictive value; * Child Health and Development, Maternal
and Child Health and Family Planning, Geneva, 1992. |
Development Screening Tools of the Future
Two promising screening tools may become available
for use in the near future. The first – Guide for Monitoring Child
Development (GMCD) – is a parental report-based development monitoring
tool for children between 0 to 3.5 years originally developed in Turkey
[8]. It comprises of 7 items pertaining to developmental concerns, and
takes 5-10 minutes to administer. The sensitivity and specificity are
86% and 93%, respectively. It also has an intervention package that
helps in supporting normal development and managing developmental
difficulties. A five-year project ‘Development of International guide
for monitoring child development’ is currently underway in India,
Turkey, Argentina and South Africa since 2010 [5]. The aim of this
project is to standardize GMCD for universal use in children
irrespective of demographic, cultural or linguistic considerations. The
project also aims at examining an approach in which monitoring is done
at community health clinics by trained personnel.
The second new kid-on-the-block is the INCLEN
Neurodevelopmental Screening Test (NDST) that was developed by the
composite efforts of a team of neuro-developmental experts from India
and abroad. It screens for 10 neurodevelopmental disorders (NDD): Autism
Spectrum Disorders, Learning Disorder, Attention Deficit and
Hyperactivity Disorder, Vision Impairment, Hearing Impairment,
Intellectual Disability, Speech and Language Disorders, Epilepsy,
Cerebral Palsy and other Neuro-Muscular Disorders. Diagnostic criteria
(Consensus Clinical Criteria) have been developed for establishing each
diagnosis which are sequentially applied according to an algorithm when
the screening test is positive [35]. Application of the NDST in a
recently concluded multi-centric validation study in rural, urban, hilly
and tribal areas revealed that the prevalence of ≥1 NDD in children
aged 2-9 years ranged between 7.5-18.5% [36].
Developmental Screening in Office Practice
Setting up routine screening practice involves
creating parental awareness and demand, finding the right opportunity,
tool selection, acquisition and training in administration, scoring,
interpreting results and counselling. This entails planning when, where,
and how screenings will be accomplished, devising a method for
documenting observations and maintaining records, communicating results
to parents, referring to experts for further evaluation when required
and scheduling future screenings. Parents can be sensitized by
information pamphlets and office displays. Since visits for acute
illnesses are not appropriate opportunities; a practical option would be
to club screening with pre-existing scheduled visits like immunization
and vitamin A prophylaxis. A system needs to be devised to document
results, maintain and update records at subsequent visits. Comparison
with previous records helps to recognize potential developmental
problems or regression, deviancy or dissociation. Experience from other
countries has shown that time actually gets saved since it takes the
same time that would otherwise have been spent in unstructured
questioning and answering other parental queries. Ultimately evaluation
time becomes predictable, detection rate increases, parent and provider
satisfaction level increases and office attendance increases as parents
start appreciating the monitoring process.
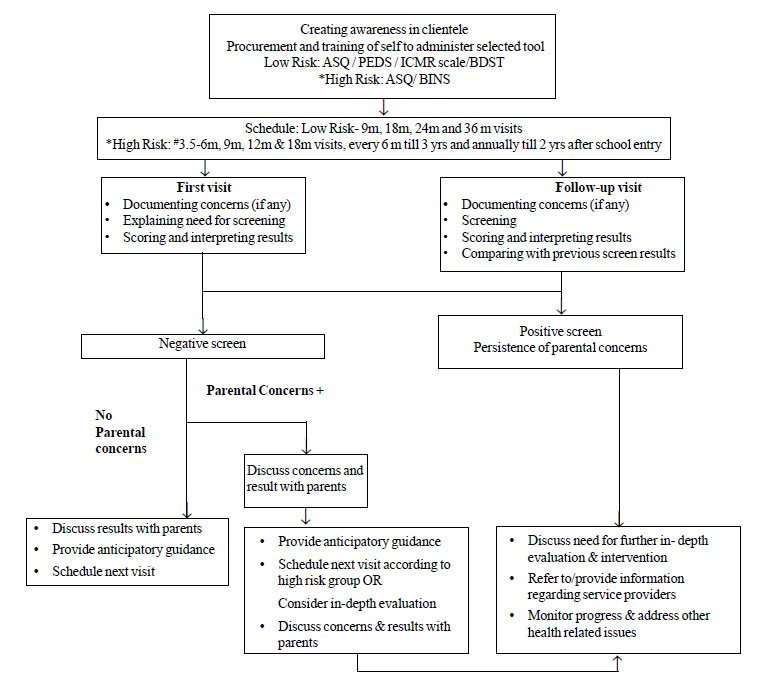
An Algorithmic Approach to Developmental Screening
Based on the advantages and drawbacks of the
tabulated tools and until consensus statements are formulated by expert
groups, the authors suggest a potential practice paradigm for
pediatricians based on degree of risk of developmental delay (Fig.
1).. Pr. Preliminary steps involve creating awareness, procuring tools
according to the type of patients encountered (low-risk, high-risk or
both), and achieving competency in administration, scoring and
interpretation. The schedule of screening and follow up monitoring will
differ according to level of risk.
 |
|
*Neonates, Infants or children with
≥1 High risk
factors viz., Genetic: positive family history of illness
associated with neurodevelopmental morbidity; Biological: acute
& chronic illnesses, nutritional (macro & micro) deprivation;
Environmental: exposure to poverty, violence, neglect,
teratogens, arsenic, lead, drugs, etc.; Psycho-social:
illiteracy, lack of stimulation, learning opportunities, poor
parenting skills, parental illness or substance abuse, maternal
depression, etc.; Presence of any parental concerns regarding
development. #Abnormality present at 3.5 months: refer to text
(discussing parental concerns & test outcomes).
Fig.1 Proposed schema of office based
developmental screening and surveillance.
|
Discussing Parental Concerns and Test Outcomes
Parental concerns should always be asked. In the
initial visit, if the parent of a low risk child expresses developmental
concerns, the pediatrician is expected to discuss these with the parents
and offer options of more frequent and earlier monitoring (as in the
high risk group) or referral for an in-depth evaluation even if the
screen is negative. If the parents opt for the former and the concerns
persist at the next visit, immediate referral is warranted. If not,
monitoring should continue as for the high-risk group, In this group,
the first visit recommended by AAP is 4-6 months (coinciding with the
2nd or 3rd immunization visit). The corresponding immunization visit in
India would be at 3.5 months. At this age, a small proportion of infants
display transient benign tone abnormalities that may be mistaken as
pathological. In these instances, the pediatrician should make a note in
the child’s records and schedule a repeat visit after a month, without
unduly alarming the parents. If it persists, in-depth evaluation would
be required.
Once screening is complete, it is important to
properly convey the significance of the results. If negative, parents
should be reassured that development is currently appropriate,
anticipatory guidance should be given about expected milestones and the
necessity of returning for the next screening visit should be explained
and scheduled. If positive, the implications need to be discussed in
depth with the parents, and they should be counseled about the need of
diagnostic evaluation and start of stimulation or intervention as
indicated post evaluation. Since parents have intrinsic faith in us as
health care providers of their children, it is our moral responsibility
to be instrumental in arranging referrals (by providing contact details
or direct communication) as well as providing continual medical help and
moral support. It is good practice to develop a two-way communication
system with service providers to instill confidence in parents regarding
management issues.
Screening should be considered the initial step of
intervention services [37]. Unfortunately, it is common practice to
falsely reassure or delay referral to alleviate parental anxiety. Actual
practice should be ‘Refer not defer.’ Failing to refer for diagnosis and
intervention after detection on screening is considered unethical [38].
In developed countries, a referral rate of 1/6 children screened is
considered optimal [39]. It is important to understand that starting
multi-disciplinary intervention (speech and language therapy,
occupational therapy, physical therapy, special educational services,
etc) should proceed in parallel to diagnosis-establishment and not
afterwards. In addition to formal intervention, pediatricians must
become familiar with home-based intervention strategies that should be
shared with the parents. Development oriented packages have been
combined with tools like ‘Integrated Management of Child Illnesses –
Care for Development’ (WHO/UNICEF), GMCD, TDSC and Developmental
Assessment Tool for Anganwadis (DATA) or are already in practice at the
community level via National Rural Health Mission, RBSK, Integrated
Child Development Schemes, and other agencies, the details of which are
available, can be practiced by parents at home, and have been proven to
be beneficial [8,14,34,40-45].
Conclusions
Many parents and children struggle in their daily
lives due to problems arising from undetected development delay.
Considering the widespread prevalence of developmental problems, the
pediatrician must remain vigilant. By adopting developmental screening
and surveillance, one can ensure a systematic approach to children with
developmental concerns and help improve their future. Both strategies
are integral parts of child healthcare, benefit the individual child and
society, and also protect the doctor from possible future litigation. In
this review, an attempt has been made to sensitize colleagues to the
importance of screening and surveillance, compare existing screening
tools and propose those suitable for Indian children along with
strategies for incorporation into office practice. There is a strongly
felt need to develop more culturally appropriate, norm-based, valid and
reliable Indian developmental screening instruments. We strongly urge
that a consensus be formulated at the National level by experts on
appropriate developmental surveillance and screening recommendations.
Ultimately, earlier recognition of developmental delay results in better
inclusion of affected individuals in society, establishment of
prevalence data, educated health policy decisions, and resource
allocation at the Government level.
Contributors: SBM: devised the review paper
concept and will stand as guarantor. All authors helped in the
literature search and selection of articles appropriate for the purpose
of the review; SBM: drafted the manuscript with critical inputs from SA,
VK and RS. All authors approved the final manuscript.
Funding : None; Competing interests: None
stated.
References
1. Grantham-Mc Gregor S, Cheung YB, Cueto S, Glewwe
P, Richter L, Strupp B, et alelopment in developing
countries: Developmental potential in the first 5 years for children in
developing countries. Lancet. 2007;369:60-70.
2. Lynch TR, W2. Lynch TR, Wildman BG, Smucker WD. Parental
disclosure of child psychosocial concerns: relationship to physician
identification and management. J Fam Pract. 1997;44:273-80.
3. Bellman M, Byrne O, Sege R. Developmental
assessment of children. BMJ: 2013: 346;e8687.
4. World Health Organization, World Bank. World
report on disability. Geneva, World Health Organization, 2011. Available
from: URL:http://www.who.int/disabilities/world_report/2011.
Accessed January 15, 2014.
5. Krishnamurthy V, Srinivasan R. In: Childhood
Disability Screening Tools: The South East Asian Perspective. A Review
for the WHO Office of the South East Asian Region. Mumbai. WHO, 2011.
6. Dworkin PH. British and American recommendations
for developmental monitoring: the role of surveillance. Pediatrics.
1989;84:1000-10.
7. Council on Children with Disabilities, Section on
Developmental Behavioral Pediatrics, Bright Futures Steering Committee,
Medical Home Initiatives for Children with Special Needs Project
Advisory Committee. Identifying infants and young children with
developmental disorders in the medical home: an algorithm for
developmental surveillance and screening. Pediatrics. 2006;118:405-20.GN="JUSTIFY">8. Ertem IO, Dogan DG, Gok CG, Kizilates SU, Caliskan
C, Atay G, et al. A guide for monitoring child development in
low- and middle-income countries. Pediatrics. 2008;121:e581-89.
9. Macias MM, Lipkin PH. Developmental surveillance
and screening: refining principles, refining practice. How you can
implement the AAP’s new policy statement. Contemp Pediatr. 2009;26:72-76.
10. Hix-Small H, Marks K, Squires J, Nickel R. Impact
of implementing developmental screening at 12 and 24 months in a
pediatric practice. Pediatrics. 2007;120:381-9.
11. Radecki L, Sand-Loud N, O’Connor KG, Sharp S,
Olson LM. Trends in the use of standardized tools for developmental
screening in early childhood: 2002-2009. Pediatrics. 2011;128:214-19.
12. Desai PP, Mohite P. An exploratory study of early
intervention in Gujrat State, India: Pediatricians’ perspectives. J Dev
Behav Pediatr. 2011;32:69-74.
13. Persons with Disabilities (equal opportunities,
protection of rights and full participation) Act, 1995. Part II, section
1 of the Extraordinary Gazette of India, Ministry of Law, Justice and
Company affairs (legislative department). Available from: URL:
http://socialjustice.nic.in. Accessed December 27, 2013.
14. National Rural health mission, Ministry of Health
and Family Welfare, Government of India. Rashtriya Bal Swasthya
Karyakram (RBSK) Child Health Screening and Early Intervention Services
Under NRHM: Operational Guidelines. Nirman Bhavan, New Delhi. 2013.
15. Robertson J, Hatton C, Emerson E. The
identification of children with or at significant risk of intellectual
disabilities in low and middle income countries: a review. CeDR Research
Report. 2009:3
16. Fernald LCH, Kariger P, Engle P, Raikes A.
Examining Early Child Development in Low Income countries: A Toolkit for
the Assessment of Children in the First Five Years of Life. World Bank
Human Development Group. 2009
17. Lansdown RG. Culturally appropriate measures for
monitoring child development at family and community level: A WHO
collaborative study. Bull World Health Organ. 1996;74:283 90.
18. Glascoe FP, Byrne KE, Ashford LG, Johnson KL,
Chang B, Strickland B. Accuracy of Denver II in development screening.
Pediatrics. 1992;89:1221-5.
19. Glascoe FP, Byrne KE. The accuracy of three
developmental screening tests. JEI 1993; 17:268-379.
20. Frankenburg WK, Dodds J, Archer P, Shapiro H,
Bresnick PB. Denver II: A major revision of re-standardization of Denver
Developmental Screening Tool. Pediatrics 1992; 89:91-7.
21. Aylward GP. The Bayley Infant Neuro-developmental
Screener. San Antonia, Tex: Psychological Corporation 1995.
22. Macias MM, Saylor CF, Greer MK, Charles Jm, Bell
N, Katikaneni LD. Infant screening: the usefulness of the Bayley Infant
Neurodevelopmental Screener and the Clinical Adaptive Test/Clinical
Linguistic Auditory Milestone Scale. J Dev Behav Pediatr.
1998;19:155-61.
23. Bricker D, Squires J, Potter L. Revision of a
parent completed screening tool: Ages and Stages Questionnaires. J
Pediatr Psychol. 1997;32:313-28.
24. Juneja M, Mohanty M, Jain R, Ramji S. Ages and
Stages Questionnaire as a screening tool for developmental delay in
Indian children. Indian Pediatr. 2012;49:457-61.
25. Majnemer A, Rosenblatt B. Reliability of parental
recall of developmental milestones. Pediatr Neurol. 1994;10:304-8.
26. Glascoe FP. Parents concerns about children’s
development: pre-screening technique or screening test. Pediatrics.
1997;99:522-8.
27. Pritchard MA, Colditz PB, Beller EM. Parents
evaluation of developmental status in children with a birthweight of
1250 gm or less. J Paediatr Child Health. 2005;41:191-6.
28. Malhi P, Singhi P. Role of Parents Evaluation of
Developmental Status in detecting developmental delay in young children.
Indian Pediatr. 2002;39:271-5.
29. Alpern G, Boll T, Shearer M. Developmental
Profile II (DP II). Los Angeles: Western Psychological Services;1986.
30. Developmental Profile 3rd Ed. Revised and
updated. An Accurate and an Efficient Means to Screen for Development
delays. Los Angeles: Western Psychological Services;2004.
31. Phatak AT, Khurana B. Barado Developmental
Screening Test for infants. Indian Pediatr. 1991;28:31-7.
32. Vazir S, Naidu AN, Vidyasagar P, Landsdown RG,
Reddy V. Screening Test for Psychosocial development. Indian Pediatr.
1994;31:1465-75.
33. Malik M, Pradhan SK, Prasuna JG. Screening for
psychosocial development among infants in an urban slum of Delhi. Indian
J Pediatr. 2007;74:841-5.
34. Nair MK, George B, Lakshmi S, Haran J, Sathy N.
Trivandrum developmental screening Chart. Indian Pediatr.
1991;28:869-72.
35. Gulati S, Aneja S, Juneja M, Mukherjee S,
Deshmukh V, Silberberg D, et al. INCLEN diagnostic tool for neuro-motor
impairments (INDT-NMI) for primary care physicians: Development and
validation. Indian Pediatr. 2014;51:613-9.
36. Silberberg D, Arora N, Bhutani V, Durkin M,
Gulati S. Neuro-developmental disorders in India – An INCLEN study.
Neurology. 2013;80:IN6-2.001.
37. Early Headstart National resource Centre.
Developmental Screening, Assessment and Evaluation: Key Elements for
Individualizing Curricula in Early Headstart Programs. Available from
http://www.zerotothree.org. Accessed December 27, 2013.
38. Perrin E. Ethical questions about screening. J
Dev Behav Pediatr. 1998;19:350-2.
39. Glascoe FP. Screening for developmental and
behavioral problems. Dev Disabil Res Rev. 2005;11:173-9.
40. Department of Child and Adolescent Health
Department, WHO. IMCI Care for Development. Available from:
http://www.who.int/maternal_child_adolescent health. Accessed
November 19, 2013.
41. Nair MKC, Russell PS, Rekha RS, Lakshmi MA, Latha
S, Rajee K, et al. Validation of Developmental assessment Tool
for Anganwadis (DATA). Indian Pediatr. 2009;46:S27-35.
42. D. Landis, J.M. Bennett, M.J. Bennett, editors. Handbook
of Intercultural Training. 3rd ed. Thousand Oaks, CA: Sage
Publications; 2004.
43. Nair MKC. Early stimulation CDC Trivandrum Model.
Indian J Pediatr. 1992;59:662-7.
44. Nair MKC. Early Child Development - Kerala Model.
Global Forum for Health research, Forum 3 Geneva: WHO 1999.
45. World Health Organization, UNICEF. Counsel the
Family on Child Development-Counseling Cards. Available from:
http://www.unicef.org/earlychildhood. Accessed December 27, 2013.
|

