Acute exacerbations of asthma are an important cause of morbidity, school absenteeism and frequent visits to the clinic or hospital. There is enough data globally to prove that the prevalence and severity of asthma is increasing(1-4). There has been an increase in mortality as well, particularly in younger age groups(5-8). For proper management of acute asthma, it is essential to follow set guidelines. This article incorporates the guidelines given by International consensus groups and also suggests alternative therapies.
Definition
Acute exacerbations of asthma are acute episodes of progressively worsening short- ness of breath, cough, wheezing, chest tightness or a combination of these symptoms. An acute severe exacerbation of. asthma that does not respond to conventional therapy is called status asthmatics.
Management of an Acute Attack of Asthma
The following steps may be useful in
planning the treatment protocol for a child
with an acute attack of asthma.
Step
1.
Assessment of severity of attack.
Step
2.
Initial bronchodilator therapy and
treatment of hypoxia.
Step
3.
Assessment of response to therapy and modification of therapy.
Step
4. Intensive care and ventilation in
refractory cases
Step 1. Assessment of Severity
Initial assessment is necessary to rapidly determine the degree of airway obstruction and hypoxia. One can immediately identify severe or life threatening cases and give these patients vigorous therapy even before going for detailed
assessment.
The features of a life threatening attack are: (i) Cyanosis, silent chest or feeble respiratory effort; (ii) Fatigue or exhaustion; and (iii)
Agitation or reduced level of consciousness.
Any child with features suggestive of a life threatening attack should ideally be treated in a hospital where intensive care facilities are available. Enquiries should be made about availability of a bed and child transferred as quickly as possible after initiation of oxygen and inhalational therapy with the help of nebulizer or MDl and spacer, the same being continued on the way.
Clinical Assessment
In case the child does not have a very severe attack of asthma, a detailed assessment is done based on history, physical examination and objective measurement of the degree of airway obstruction and hypoxia.
History
Once an appropriate level of management has been instituted in a sick child, a detailed history should be taken with emphasis on certain points. It is necessary to know the duration of worsening and any specific allergen or irritant which could have triggered the attack, any history of previous hospitalizations, frequent emergency visits, chronic corticosteroid use or recent withdrawal from systemic steroids and history of previous admissions to intensive care unit or intubation. These factors, if present, increase the risk of the attack becoming very severe and such children should be intensively monitored.
Physical Examination
The initial examination Should rapidly determine the severity of airflow obstruction,
degree of hypoxia, and identify complications. Categorization of an acute exacerbation of asthma into mild, moderate or severe can be done based on physical examination and objective parameters as shown in Table I. In any child with severe degree of respiratory distress, presence of alteration of sensorium, confusion, and cyanosis will suggest respiratory failure. Examination should be repeated after each step of treatment to assess the response.
Objective Assessment
Many patients may not perceive any distress even when they have moderate degree
of airway obstruction. More importantly, even when symptoms and physical signs are minimal, the patient may have considerable degree of airflow obstruction. An objective measurement of lung function thus becomes necessary. The two methods of objective measurement of lung function that can be used are: (i) measurement of air flow obstruction by peak expiratory flow rate (PEFR) or forced expiratory volume in the first second (FEV1) and (ii) arterial
blood gas analysis (ABG) or pulse oximetry.
In children who are very young
<
5
yrs) or those who are very sick, arterial blood gas analysis or pulse oximetry should be used to assess the response to therapy and take a decision to transfer the child to intensive care unit.
Chest Radiograph and Other Laboratory Studies
Laboratory studies are generally not indicated in a routine acute exacerbation. However, if the child is unusually ill or there is a doubt of an infection, blood samples can be taken for: (i) white blood cell count for detecting polymorphonuclear leukocytosis and bandemia which suggests bacterial infection, (ii) serum electrolytes, since both beta 2 agonists and corticosteroids may cause hypokalemia, and (iii) serum theophylline levels (if facilities are available). If the child is already on theophylline, levels may be necessary before institution of the same by intravenous. route, as it has a very low safety margin.
A chest radiograph is indicated only where the diagnosis is in doubt or there is a suspicion of a foreign body. It is also useful in a child with high grade fever, localized crepitations, decreased breath sounds and any other finding suggestive of infection or complications like pneumothorax, atelectasis and pneumomediastinum.
Step 2. Initial Therapy
Principles of Therapy
* The goal is to rapidly reverse the acute airflow obstruction with consequent relief of respiratory distress. This is achieved by repeated use of inhaled beta-2 agonists.
* Hypoxia is treated by proper oxygenation of all acutely sick children.
* Corticosteroids are added early in an acute attack, particularly if the response to inhaled bronchodilators is not satisfactory.
*
Repeated clinical and objective assessment is done to evaluate the
response to the above and also to detect impending respiratory failure at the earliest. Other drugs are added if necessary.
TABLE I
Estimation of Severity of Acute Exacerbation of Asthma
|
Sign/Symptom |
Mild |
Moderate |
Severe |
|
Respiratory rate
|
Normal
|
Increased |
Increased |
|
Alertness |
Normal
|
Normal
|
May be decreased |
|
Dyspnea |
Absent or mild; speaks in complete sentences |
Moderate; speaks in phrases or partial sentence
|
Severe; speaks only in
single words
or short phrases |
|
Pulsus paradoxus |
< 10 mm Hg |
10-20 mm Hg |
20-40 mm Hg |
|
Accessory muscle use |
No intercostal
to mild retriactions |
Moderate intercostal retraction with tracheosternal retractions, use of sternocleidomastoid muscle |
Severe Intercostal and tracheosternal
retraction with nasal flaring
|
|
Color
|
Good |
Pale |
Possibly cyanotic |
|
Auscultation |
End expiratory wheeze only |
Wheeze during entire expiration and inspiration |
Breath sounds becoming inaudible |
|
Oxygen saturation |
>95% |
90-95% |
<90% |
|
paCO2 |
< 35 mm Hg |
<40mg Hg |
> 40 mm Hg |
|
PEFR |
70-90% of predicted or personal best |
50-70% of predicted or personal best |
< 50% of predicted or personal best |
PEFR-Peak expiratory flow rate.
Initial Therapy
Oxygen
All patients of acute severe asthma have some degree of hypoxia. Oxygen at the rate of 3-6 liters/minute should be started. The flow should be enough to maintain oxygen saturation above 92%.
Beta-2 Agonists
The currently recommended standard broncholidator therapy is repeated inhalation of beta-2 agonist aerosol. Salbutamol nebulizer solution (5mg/ml) in the dose of 0.1-0.15 mg/kg diluted in 3 ml of normal saline is administered over a period of 10-15 min. It is
preferable to use central oxygen supply at the rate of 6-7 L/min to run the nebulizer, at least initially, to avoid hypoxia. The dose can be repeated every 20 min for three times and the child reassessed after that. The rationale behind giving repeated doses of inhaled bronchodilators is that the bronchodilation that follows the initial dose allows more distal deposition of drug particles during further
dosing. This results in dilation of smaller airways and the short dosing interval prevents any deterioration of clinical status in the intervening period(9). Recent studies however suggest that continuous nebulization (CN)
may be more effective than intermittent nebulization(10-12). This: method of therapy can continue for prolonged periods without having to set up nebulization at regular intervals. Also patients are more likely to get acclimatised to CN and therefore maintain a more constant breathing pattern.
This would result in subsequent reduction of inspiratory flow and more peripheral deposition of inhaled
bronchodilator aerosol(13). Recommended
doses are 0.1-0.5 mg/Kg/h via a delivery system comprising preferably of an infusion pump and central oxygen supply. Higher doses of 3.4
±
2.2 mg/Kg/h have been used in ventilatedpatients(12,14). This set up is difficult to maintain, since it requires power and oxygen supply for prolonged periods. However, the last word on superior efficacy of CN over intermittent nebulization has not yet been said.
Alternatively, metered dose inhaler (MDI) can be used with a spacer device to give repeated inhalations of beta-2 agonist. It is considered equivalent(4) or better(15) than nebulizer driven by compressed air. It does not cause oxygen desaturation unlike the former. The duration of therapy is less than a minute as compared to 15 minutes with a nebulizer. Use of MDI reduces the cost of the therapy, is easily performed. and does not require power supply. One to two puffs every 5-10 min can be used for 10-20 times(16). One can use a commercially available large volume (750 ml) spacer device. However, if this is not available, any plastic bottle of about one litre
capacity cut at the bottom for introduction of mouthpiece of inhaler can also be used. The mouth of the bottle can be cut and widened
appropriately to cover the mouth and nose of the baby like a mask.
In some children with severe bronchospasm, an initial dose of epinephrine may be helpful prior to initiating inhalational therapy(17). Oxygen desaturation seen with nebulization therapy is not seen with this form of therapy. On the contrary transient increase in
PaO2 has been noticed by some workers(18,19). Use of epinephrine is limited by it's shorter duration of action, cardiac side effects and it can not be repeated more than 2-3, times. Injection terbutaline may also be used in place of epinephrine. It has a longer duration of action and repetition of dose is not required for 2-6 hours.
Anti-cholinergics
Some studies have shown that concomitant use of inhaled anticholinergics and a selective beta-2 agonist 'produces significantly more improvement in lung function than beta-2 agonist alone(20,21). Only, ipratropium bromide is used in view of negligible side effects(22). Transient. aniscoria
and angle closure glaucoma have been noticed in adults(23,24).
Recent consensus protocols(25,26) suggest institution of nebulized ipratropium as part of immediate treatment, if life threatening features are present. It may also be added later, if reassessment shows poor or partial response to initial therapy with beta-2 agonists.
Parasympathetic fibres are present in larger airways, in contrast to beta adrenergic receptors, which are located in more peripheral airways. Ipratropium may also have a generalized action throughout the lung(27). It is an acetylcholine antagonist while salbutamol
is a beta-2 agonist, both act at different sites in the lung and
via different pharmacologic mechanisms, which provides the basis for using these drugs
together. There are however, some studies which have shown no benefit of using anti- cholinergic drugs(28,29).
An optimal dose of 250
µg (30) which is present in 1.0 ml of the respirator solution, may be mixed with salbutamol solution and both given together at an interval of 20 minutes with the nebulizer. It may also be given alternating with the dose of nebulized salbutamol. Dosing frequency may be reduced as the patient improves.
In patients who suffer from tachycardia or marked tremors in response to standard dose of beta-2 agonists and in younger age group (3-30 mo) this agent may be more effective than salbutamol(31,32).
Corticosteroids
Since inflammation is an important component of airway compromise
in an acute attack of asthma, there is no doubt that the use of
steroids in an exacerbation is useful in resolving the
obstruction(33,34), but it is somewhat difficult to decide precisely when steroids should be administered. It has been proved in both adults and children(35,36) that steroids given for a short duration of 3-7 days, improve the resolution and reduce the chances of an early relapse. However, the important questions that remain to be answered are that does every child require a short course of steroids, even when the exacerbation is mild or moderate, and if so, how many such courses can safely be given when the child continues to get acute exacerbations despite an attempt to improve the prophylactic therapy?
It is evident that the timing of initiation of steroid therapy
plays a major role in the subsequent outcome of the attack.
Studies have shown that the efficacy of steroid therapy is most when they are started soon after the patient presents in the emergency
room(37-40). In contrast, benefits were minimal when steroids were initiated 24-48 hours after observation(41,42). A single dose of I/M methyl prednisolone
in the dose of 4 mg/kg, when given as an early adjunct to the
beta-2 adrenergic therapy has been reported to reduce the hospitalization rates(43). Indications for starting steroids at the outset may be: (i) A child with a severe or very severe attack of asthma; (ii)
Previous history of life threatening attack or severe attacks not
responding to bronchodilators; and (iii) If the child is on oral steroids or high doses of inhaled steroids for prophylaxis.
All other children can be reassessed after the initial bronchodilator therapy and
children with poor response, partial response or early relapse can be put on steroids. An oral dose of 1-2 mg/kg of prednisolone
may be as effective as an equivalent dose of hydrocortisone given
intravenously, because the time for onset of action is the same.
The total duration of therapy can be 3-7 days depending upon the
response. However children who have already been on long term oral
steroids would require a longer course with tapering of doses over 5-10 days. New guidelines however, advise to use initial dose of steroids in every attack that is of moderate or more severity(25,26).
Aerosolized steroids were earlier found to be ineffective in an acute attack of asthma but now there are reports(44) suggesting that nebulized dexamethasone may be quicker acting than oral prednisolone.
Step 3. Assessment of Response to Initial Therapy
Close monitoring for detecting signs of improvement or deterioration is important. The patient should be assessed after initial therapy of 2-3 doses of bronchodilator along with oxygen over a period of one
hour. The plan for further management. will depend on whether the response to initial therapy has been good, partial or poor.
Good Response
The subject with good response to initial therapy will become free of wheeze and have no breathlessness. Auscultation of chest will show minimal or no rhonchi and PEFR or FEV1 will improve to more than 70% of the predicted or personal best. Such a child can be observed in the emergency room for 2-4 hours and if remains stable, can be discharged on bronchodilators (inhaled or oral) for a period of 5-7 days. The parents should be advised to come for follow up and all other necessary "instructions should be given for prophylaxis.
Partial Response
A child may show some response after initial therapy but may still
have breathlessness and wheezing, though less. Physical examination will reveal persistence of rhonchi. PEFR will be between 40% to 70% of the predicted normal. Treatment of a child with partial response is discussed later.
Poor Response
If there is no subjective or objective improvement after initial therapy, it indicates a poor response. This child will continue to have severe respiratory distress and wheeze. Physical examination will reveal severe airway obstruction as indicated by significant pulsus paradoxus, use of accessory muscles and extensive rhonchi.
Continuation of Therapy (At the end of. One Hour)
Oxygen and Bronchodilator Therapy
If the response to the initial therapy is partial or poor, oxygen and beta-2 agonist inhalation should be continued. The frequency of inhalation should be decided according to the severity of respiratory distress. Children who do not have severe respiratory distress and have shown partial response may only require 2-4 hourly inhalation while children with severe distress should be given more frequent inhalations. Inhalation as frequently as every 20 min, or even continuous, can be given without side effects for the next two hours and child reassessed. Ipratropium if not used at the onset is added at the end of first hour as described earlier. MDl
with a spacer can also be used frequently as an effective alternate device.
Corticosteroids
Use of oral prednisolone or systemic hydrocortisone gives similar results. If not administered at outset and response at end of one hour is poor or partial, prednisolone (1-2 mg/kg oral) or hydrocortisone (10 mg/kg intravenous) may be given as an initial bolus. Corticosteroids may be continued as 0.25-0.5 mg/kg/ dose of prednisolone or 2.5-5 mg/kg/ dose of hydrocortisone, 6 hourly.
Intravenous Fluids and Correction of Acidosis
Children admitted with an acute severe attack of asthma often have mild to moderate dehydration. Dehydration may produce more viscous mucus, leading to bronchiolar plugging(45). Humidification of inspired air and correction of dehydration, there- fore, are always indicated. However, at the same time, inappropriate antidiuretic hormone secretion has been reported in some cases of bronchial asthma. Hence fluid therapy should be individualized to keep the child in normal hydration.
Hypokalemia has been reported with frequent beta adrenergic therapy(46). It should be corrected when present.
Metabolic acidosis that occurs in an
acute attack may decrease the responsive- ness to bronchodilators. It has been recommended that if pH is less than 7.3 or base deficit is greater than 5 meq, intravenous correction with sodium bicarbonate is indicated, initially using half the calculated correction and then repeating the ABG.
Monitoring
If the child is very sick and is deteriorating, he may require continuous monitoring. Repeated assessments are necessary at least at hourly intervals, in less sick children. PEFR or FEV1, wherever possible, and ABG in younger and very sick children should also be done for an objective evaluation.
If the patient has improved with continuation of the above therapy
for about two hours, he can be observed for few hours and then
discharged with proper advice. In case there is no improvement,
treatment is intensified with addition of other drugs and the child transfered to a place where intensive care facilities are available.
Addition of Other
Drugs
Role
of Aminophylline
The role of aminophylline in an acute attack of bronchial asthma is still not clear. There is no doubt that methylxanthines have bronchodilator activity but it is uncertain whether this adds to the bronchodilator effect achieved by beta-2 agonists and corticosteroids.
In a meta analysis of 13 controlled trials of intravenous aminophylline in acute asthma, no benefit of routine addition of aminophylline
to inhaled beta-2 adrenergic and corticosteroids was documented.
It has been proved in adult studies that aminophylline does not have additional bronchodilator effect(47,48). In addition methylxanthines have a very low therapeutic index
and side effects can be numerous and serious.
However, in a double blind placebo controlled trial on
hospitalized children a clear benefit was demonstrated(49). Until
further studies are carried out, aminophylline remains an adjunct
to first line beta agonist therapy in children and can be added in
a child who has not shown good response to initial therapy(25). It
is believed that aminophylline may act by mechanisms other than bronchodilation as well, such as stimulation of the respiratory drive, reduction in respiratory muscle fatiguability and enhancement of mucociliary clearance(50).
A bolus dose (5-6 mg/kg) depending upon previous treatment with
methylxanthines is given followed by infusion of maintenance dose (0.9 mg/kg/h). The dose of theophylline is reduced in fever by 50% (33), and 25-30% with various drugs like erythromycin, aminoquinolones, cimetidine and related drugs. It may have to be increased in children getting drugs like rifampicin, phenytoin and phenobarbitone. If facilities are available drug levels are mandatory to ensure safety and efficacy.
As soon as the patient shows response, aminophylline infusion may be substituted by injection deriphylline (6 hourly bolus) or even oral theophyllne if patient is able to take orally.
Intravenous Terbutaline
In children with low inspiratory rates where nebulization of beta-2 agonists has failed, intravenous terbutaline infusion, has been tried(51,52). Therapy is started with an initial bolus of 10
µg/kg
over 30 minutes, followed by an infusion at the rate of 0.1
µg/kg./min which may be increased by 0.1
µg/kg/min every 30 minutes upto a maximum of 4
µg/kg/min(53) or until
there is a fall in paCO2 with clinical improvement. Dose of terbutaline should be reduced by half(54), if theophylline is used concomitantly. Significant adverse effects noted with intravenous terbutaline are tachycardia, arrhythmias, hypertension, myocardial ischemia, hyperglycemia, hypokalemia, rhabdomyolysis, lactic acidosis and hypophosphatemia(55).
Magnesium Sulphate
Some patients with acute severe asthma, treated with intensive initial nebulization therapy with beta-2 agonists and corticosteroids may not improve and progress to respiratory failure. One drug which may be worth trying in these refractory patients, to avert mechanical ventilation, is magnesium sulphate. Although there are very few controlled trials in children using this drug, a recent double blind placebo controlled trial(56) suggests that early institution of intravenous magnesium sulphate along with conventional therapy may result in early relief of airflow obstruction.
It acts by counteracting calcium mediated smooth muscle contraction, through its influence on calcium homeostasis(57), inhibition of acetylcholine release(58) at the neuromuscular junction, inhibition of histamine release(59), direct inhibition of smooth muscle contraction(60) and sedation(61). The recommended dose for infusion is 30-70 mg/kg over 20-30 minutes(62). It is available as a 50% solution, 0.2 ml/kg of which can be given as an infusion in 30ml N/5 normal saline in 5% dextrose over 30 minutes(56). Serum levels greater than 4mg/dl are necessary for bronchodilation. Onset of action occurs within a few minutes of intravenous infusion
and lasts for 2 hours(63,64). Side effects are transient sensation
of facial warmth, flushing, malaise and hypotension. At serum levels greather than 12.5mg/dl side effects like arreflexia, respiratory depression and arrythmias may be noted, but this requires administration of doses greater than 150 mg/kg(62-64). Thus, it may be used as an adjunct to beta-2 agonist therapy, though its exact place in treatment of acute asthma remains to be determined.
Role
of Antibiotics
Respiratory tract infections that trigger exacerbations of asthma are usually viral. Bacteria and mycoplasma may be infrequently associated. Role of antibiotics, hence, is limited to: (i) patients who are running high grade fever, look sick, and toxic; (ii) sputum is purulent with presence of polymorphs and not eosinophils; and (iii) chest radiograph shows a consolidation. In all other cases, even if steroids are used, there is no need to add antibiotics.
Role
of Antihistaminics, Mucolytics, Cough
Syrups, and Sedatives
Older antihistaminics possessed relatively weak antihistaminic action and caused
more sedation. In contrast newer non-sedating, more potent H-l
receptor antagonists appear to achieve more effective histamine blockade. Astemizole inhibits bronchoconstriction in early asthmatic attack. Recent studies quote significant reductions in symptom severity and bronchodilator use, with concomitant use of these drugs(65). Azelastine, another new antihistaminic has been shown to partially inhibit bronchoconstriction in allergen- induced late reaction of atopic asthma, possibly by suppressing the release of additional inflammatory mediators(66,67). At present therefore, there is no general contraindication
to the use of antihistaminics in asthamatic patients; in fact they may be useful adjuncts to asthma therapy.
There is no evidence that addition of mucolytics and cough syrups, is in any way helpful to the patient with acute asthma. Sedation may be harmful in patients who are anxious and irritable because of hypoxia,
and should be avoided. Instead measures to treat hypoxia should be
made more effective. Occasionally younger infants may cry excessively due to reasons other than hypoxia, like hunger and unknown
surroundings. This may increase the oxygen demand and also make
management more difficult. The best way is to treat these children in the lap of mother. Rarely sedation may be required and chloral hydrate or triclofos are safe drugs for this purpose.
Step 4. Intensive Care Management
Indications for Transfer to Intensive Care Unit
The patient is observed on above therapy for next few hours and is monitored frequently. The decision to transfer to Intensive Care Unit (ICU) will depend upon the status of the child at the time of presentation and response to therapy. Any child with signs of life threatening attack, should immediately be transferred to the ICU. If the child has been receiving therapy and has shown poor response after being observed for a few hours or develops clinical signs of impending respiratory failure like persistent hypoxemia, exhaustion or change in level of sensorium, he/she also warrants transfer to ICU. Continuous monitoring with the help of pulse oximetry or repeated ABG
analysis is therefore mandatory since most of these patients may not be in a position to do PEFR.
Continuation of Therapy in ICU
The focus of care continues to be close observation and delivery of frequent nebulized beta-2 agonists, combined with corticosteroids and possibly aminophylline.
As mentioned earlier, a trial of intravenous terbutaline and magnesium sulphate, if not given so far, can be given in a child who has not responded to above therapy due to low inspiratory flow rates.
Intubation and Controlled Ventilation
Despite maximal pharmacologic therapy, some children do not respond favorably and require intubation and mechanical ventilation. The decision to ventilate is usually reserved as a last option.
Indications for Mechanical Ventilation(55) These include:
(i) Failure of maximal pharmacologic therapy.
(ii) Cyanosis and hypoxaemia (PaO2 less than 60 mm Hg).
(iii) PaCO2 greater than 50 mmHg and rising by more than 5 mmHg/h
(iv) Minimal chest movements.
(v) Minimal air exchange.
(vi) Severe retractions.
(vii)
Deterioration in mental status, lethargy or agitation.
(viii) Recumbent and diaphoretic patient.
(ix) Pneumothorax or pneumomediastinum.
(x)
Respiratory or cardiac arrest.
ABG values alone are not indicative of the need for mechanical ventilation and should be interpreted in context of the clinical picture. Frequently, more than one of these indications are present before the decision to ventilate is made. However, it must be stressed that inspite of being aware of the morbidity that ventilation entails, it is better to intubate a child electively rather than waiting for cardiorespiratory arrest to occur.
The patient should be stabilized using 100% oxygen administered by bag and mask, oral and airway secretions should be cleared and stomach decompressed using nasogastric tube, to diminish risk of aspiration. Pre-medication with intravenous atropine and topical anesthesia to hypo- pharynx and larynx, helps to decrease bronchospasm and laryngospasm, which may be produced as a result of upper airway manipulation. An ideal sedative that may be used for intubation is intravenous ketamine in the dose of 1-3 mg/kg. The largest recommended endotracheal tube should be used. Muscle relaxation eliminates ventilator-patient asynchrony and improves chest wall compliance. It reduces
PaCO2 for any given level of minute ventilation. Additionally, this gives the patient with respiratory muscle fatigue, a period of desperately needed rest. Vecuronium
bromide, with an intermediate duration of action and without any cardiovascular or autonomic side effects, in a dose of 0.2-0.3 mg/kg may be used. Succinylcholine
may be used too but has a short duration of action. A volume cycled ventilator is recommended with low respiratory rate (8-12 per min) and long expiratory time (1 : E ratio of 1 : 4 or 1: 3) since this prevents hyperinflation. Airway obstruction in itself causes intrinsic PEEP, therefore end expiratory pressure (PEEP) should be minimal. Tidal volume of 10-12 ml/kg and peak airway pressure less than 40-50 cm of water should be maintained. High inspiratory flow rates should be kept to improve gas exchange. This can usually be achieved with heavy sedation or muscle relaxants. Throughout ventilation, beta-2 agonists are nebulized into the inspiratory circuit of ventilator.
In the ventilated patients, therapeutic bronchoscopy with lavage using saline,
sodium bicarbonate and acetylcystine(68,69)
has been used in very ill patients with persistent mucus plugging, to prevent atelectasis and nosocomial pneumonia.
Role of Droperidol
Dyspnea promotes anxiety, which may impair ventilation and interfere with maximally effective use of aerosol therapy. Therefore in Pediatric lCU set up, one may use sedatives with bronchodilator proper- ties. Droperidol
which has both these properties may be used in ventilated asthmatics, who also require sedation. It antagonises bronchoconstriction mediated by alpha- adrenergic receptors in peripheral airways. Recommended dose in adults is 0.22 mg/kg(70). The main side effect noted at this dose has been hypotension.
Role of Ketamine
This drug is a disassociative anesthetic with excellent sedative and analgesic
properties. It relaxes smooth muscle directly, increases chest wall compliance and also decreases bronchospasm in ventilated asthmatic children. It is given as a loading dose of 0.5-1.0 mg/kg, followed by an infusion of 1.0-2.5 mg/kg/h in ventilated children(71). Side effects commonly encountered are arrythmias, increased secretions and laryngospasm. It has been used in sub- anesthetic doses in non-ventilated adults in lCU setup in the dose of 0.75 mg/kg bolus dose over 10 minutes, followed by an infusion
at a rate of 0.15 mg/kg/h(72). Thus intravenous ketamine can be used to relieve acute intractable bronchospasm, provided expert anesthetic help is available at hand.
ECMO
The use of extra corporeal membrane oxygenation (ECMO) as a therapeutic option(73,74) in resistant severe asthma for carbondioxide removal has been reported. Whether this has any role or not is still unclear.
Heliox
Helium oxygen mixture has been used to reduce air viscosity and treat upper airway
obstruction. Though there are no controlled trials published,
some(75) have reported a return of normal blood gases following
this treatment in patients with alveolar hypoventilation due to severe acute asthma.
Inhaled Anesthetic Agents
In patients who fail to improve with mechanical ventilation, with
beta-2 agonists continuously delivered through ventilator tubing, a trial of inhaled anesthetic gases may be given. Use of halothane 1-1.5%(76,77), isoflurane 1 %(78) and ether(79) have been seen to produce significant improvement within 1 hour. The same could be discontinued within. 12 hours, though some patients require extended therapy. The exact mechanism of action of anesthetic agents is unclear. They may relax airway smooth muscle directly(80), inhibit the release of bronchoactive
mediators, or inhibit vagal induced bronchospasm. Halothane, it is suggested, has an action similar to beta agonists(81). Administration of anesthetic agents can be done by fitting a standard ventilator with an anesthetic gas vaporiser.
The patient may be followed up by pulse oximetry and serial blood gas analysis. A high
PaCO2 may be tolerated as long as pH and oxygenation is maintained (per- missive hypercapnia), thus keeping up- ward revision of ventilator settings to a minimum. The resolution of bronchospasm in ventilated asthmatic patient will become evident when
PaCO2 values fall, while the same or lower peak airway pressure are being used. Once the
PaCO2 is less than 45 mm Hg, the peak airway pressure less than 35 cm water and there is mild or no bronchospasm on auscultation, the muscle
paralysis can be stopped. As soon as respiratory muscle function returns to normal, the patient can be placed on spontaneous ventilation. If the child can maintain a
PaCO2 of less than 45 mm Hg without assisted ventilation, extubation may be safely done.
Management During Recovery Phase and Advice at Discharge
During the recovery phase of acute asthma, the frequency of inhalation should be reduced gradually, and oral drugs should be instituted in place of intravenous medication. The patient can be discharged once symptoms have cleared and lung functions stabilized (PEFR
>75% predicted). Bronchodilator therapy consists of oral or inhaled beta-2 agonist depending upon the age of the child and affordability, and a theophylline (preferably long acting). The
instructions to the parents and the child regarding the importance of correct timing of
the drugs and proper inhalation techniques are of utmost
importance. The child should be called for follow up to detect any
early relapse and observe the medication techniques. The parents
must be told to monitor the child's symptoms and wherever
possible, objective measurements like PEFR should be recorded to detect any worsening.
Prevention of Future Asthma
The following points must be. kept in mind to prevent future exacerbations of asthma(82):
(i) Parents of children should be given proper education regarding home
management of asthma. They should be provided with written
instructions regarding the administration of drugs during acute
asthma episode, and taught how to recognize deteriorating control,
both clinically and by measurement of PEFR in older children.
(xi)
Parents should know when to seek
medical help and where.
(iii) Children should be supervised regularly.
(iv) A proper prophylactic therapy should be planned depending upon the age and affordability. A child who has suffered from a very severe attack will generally require inhaled steroids.
(v) Simple methods of delivery like MDl with space (home made or commercial) should be made available to as many patients as possible.
(vi) Hospitals should follow written protocols giving clear guidelines of
management for acute as well as chronic asthma.
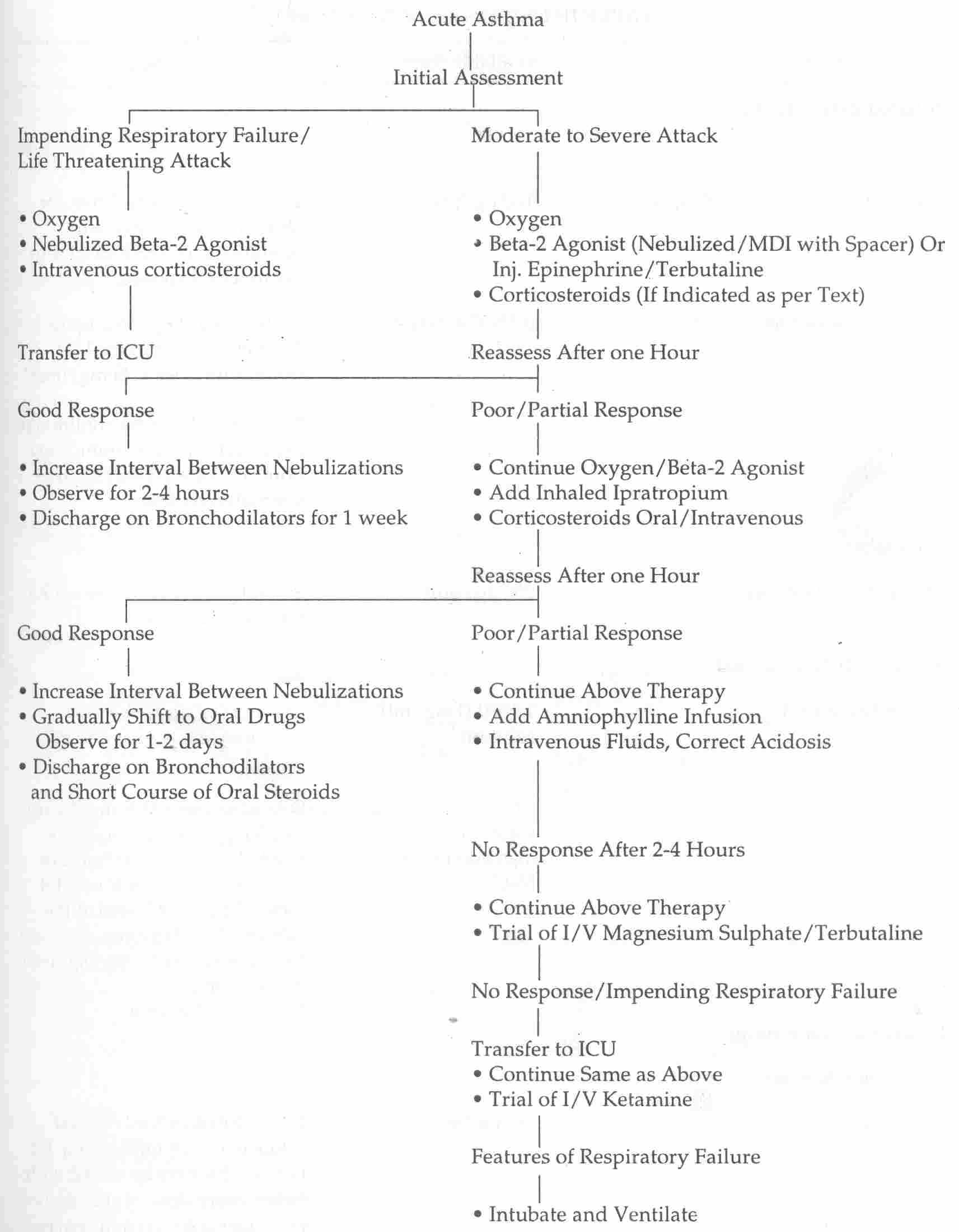
An algorithm for the management of acute asthma is depicted in Fig. 1 and
the recommended drug dosages are summarized in Table II.
 |
|
Fig. 1.
Algorithm for Management of Acute Asthma |
TABLE II
Drug Dosages in Acute Attack
|
Drug |
Available form |
Dosage |
|
Inhaled beta-2 agonist |
|
|
|
Salbutamol |
|
|
|
Metered dose inhaler with spacer |
100
µg/puff |
2 inhalations every 5 min for total of 10-20 puffus, with monitoring of PEFR or FEV to document response. |
|
Nebulizer solution |
0.5% (5mg/ml) |
0.1-0.15 mg/kg/ dose up to 5 mg every 20 min for 1-2 h (minimum dose 1.25 mg/ dose) or
0.1-0.5 mg/kg/h by continuous nebulization (maximum 15mg hour) or 3.4 :t 2.2mg/kg/h in ventilated patients. |
|
Terbutaline |
|
|
|
Metered dose inhaler |
200 µg/puff |
2 inhalations every 5 min for a total of 10-20 puffs. |
|
Systemic beta-2 agonist |
|
|
|
Epinephrine HC1 |
1:1000 (1mg/ml) solution |
0.01 mg/kg up to 0.3 mg subcutaneously every 20 min for 3 doses |
|
Terbutaline |
0.05% (0.5 mg/ml). solution for injection in 0.9%
NaCI |
Subcutaenous 0.005 mg/kg up to 0.3 mg every 2-6 hours as needed. Intravenous bolus of 10
µg/kg over 30 minutes followed by IV infusion at the rate of
0.1
µg/kg/min. Increase as necessary by
0.1
µg/kg/min every 30 min. Max.4
µg/kg/min. |
|
Inhaled anticholinergics |
|
|
|
Ipratropium Bromide |
|
|
|
Nebulizer solution |
250µg/ml |
1 ml diluted in 3 ml normal saline every 20 minutes for 1-2
hours. This may be mixed with either every dose of slabutamol nebulizer solution or alternated with salbutamol. |
|
MethxIxanthines |
|
|
|
Aminophylline |
80% anhydrous theophylline 250 mg/10 ml injection |
If no previous theophylline use, load with
5-6 mg/kg and maintain at 0.9 mg/kg/hr. If previous theophylline given,
no bolus |
|
Corticosteroids |
|
|
|
Prednisolone |
5,10,20 mg tabs |
1-2 mg/kg/dose every 6 h for 24 h then 1-2
mg/kg/day in divided doses every 8-12 hours |
|
Hydrocortisone |
50 mg/ml injection |
10-20 mg/kg/24 h in 4 divided doses |
|
Methylprednisolone |
40 mg/ml injection |
4 mg/kg IV single dose |
|
Magnesium Sulphate |
50% soln. for injection (500 mg/ml) |
30-70 mg/kg in 30 ml N/5 saline intravenous infusion over 30 minutes. |
