A. Sood
D. Sama
R. Sharma*
S. Rastogi**
From the Departments of Endocrinology and
Meta-bolism, Radiodiagnosis* and Orthopedics**, All India
Institute of Medical Sciences, New Delhi 110 029, India.
Reprint requests: Dr. Ajay Sood, Assistant
Professor, Department of Endocrinology and Metabolism, All India
Institute of Medical Sciences, New Delhi 110 029, India.
Manuscript Received: August 19, 1999;
Initial review completed: September 21, 1999;
Revision Accepted: October 18, 1999
Metaphyseal chondrodysplasia previously known
as metaphyseal dysostosis, is a rare autosomal dominant disorder
of endochondral ossification, characterized by accumulation of
cartilage in various skeletal sites, specifically metaphysis of
tubular bones(1). Twenty cases of Jansen’s metaphyseal
chondrodysplasia had been reported till 1994(2), and subsequently
there is no case report in the Medline literature. Clinical
diagnosis is made on the basis of short stature with bowing of the
legs in newborn period or early infancy. There is marked widening
of the joints with contractures. Striking radiological changes
include expanded and cup shaped metaphysis with normal epiphysis
and diaphysis(3), Half the number of the cases may have
hypercalcemia and hypo-phosphatemia(4,5). This entity may simulate
rickets refractory to vitamin D, renal tubular acidosis, renal
osteodystrophy, hyperpara-thyroidism or hypophosphatasia(6).
Jansen’s metaphyseal chondrodysplasia has not been reported in
the Indian literature.
A female child of 6˝ years with history of
birth at 32 weeks gestation presented with early onset of multiple
bony deformities. Her birth weight was 1.5 kilograms. Nasogastric
feeding was given for the initial few weeks of her life. Widening
of wrists, knees and ankle joints, and chest deformities were
noticed at the age of one month. Her weight at ten months of age
was six kilograms. Motor development was slow. She developed joint
contractures and was not able to sit, stand or walk. Despite the
administration of calcium and vitamin D her deformities worsened.
She had fractured her left forearm at the age of two years. Other
developmental milestones were normal. She suffered from recurrent
respiratory tract infections since the age of one month. There was
no history of parental consanguinity or family history of
metabolic bone disease. Her sister had normal growth and
development.
Examination revealed that the child (Fig.1)
was thin built.
|

|
She had less than average intelligence
(Intelligent Quotient 60 to 70). Her length was 88 cm, which was
less than 2 standard deviations by Indian Council of Medical
Research standards(7). The calculated midparental height was 156.3
cms, which is 75th percentile of Indian Council of Medical
Research standards. The head circumference was 48.5 cm. She had
normal hair, skin and eyes. She had bowing of upper and lower limb
long bones, widening of wrists and ankle joints. Contractures of
left elbow, right hip and both knee joints (flexion deformities)
were present. Flexion deformities were also present at proximal
interphalangeal joints. Frontal bossing, rachitic rosary, Harrison’s
sulcus were present. The spine was normal on clinical examination.
The patient had generalized hypotonia with normal reflexes,
without any sensory nerve involvement. Rest of the systemic
examination was normal. |
| Fig.
1. Photograph of the patient showing severe deformities. |
|
Laboratory investigations revealed serum
calcium 9.3 mg/dl, phosphorus 5.6 mg/dl and alkaline phosphatase
12.9 KAU. Twenty-four hour urinary excretion of calcium was 52 mg
and phosphorus 275 mg. Hematological parameters, blood urea, serum
creatinine and serum electrolyes were normal. Her renal tubular
absorption of phosphate was 84%.
Radiological investigations: Radiographs of
the upper extremity (Fig. 2) showed marked widening and
fraying of the metaphyses of humerus, radius and ulna with an
irregular fragmented appearance.
|

|
Fig. 2. AP radiograph of the upper
extremity shows bilateral symmetrical widening, fraying and
irregular fragmented appearance of all the metaphyses with
sparing of the epiphyses.
|
|
|
Severe metaphyseal irregularity,
widening and fragmented appear-ance with diaphyseal bowing were
also seen to involve the femur, tibia and fibula (Fig. 3).
The epiphyses of the long tubular bones of both the upper and
lower extremities were bulbous. Small tubular bones (metacarpals
and meta-tarsals) showed irregular metaphyses with normal
epiphyses. Chest radiograph (Fig. 4) revealed irregular
costochondral junctions, glenoid fossae and inferior angles of
scapulae. Lateral radiograph of the dorsolumbar spine (Fig. 5)
revealed an increased height of the vertebral bodies with an ovoid
configuration, and increased density of the antero-superior and
antero-inferior margins of vertebrae. The skull radiograph was
normal. Radiographs of the patient at 2 years of age also showed
similar findings, although of less severity (Fig. 6).
|

Fig. 3. AP radiograph of the lower
extremity shows gross metaphyseal irregularity widening with
diaphyseal bowing. The epiphyses are bulbous.
|
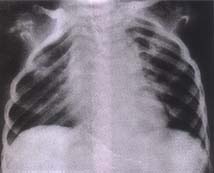
Fig. 4. Chest skiagram shows irregular
costochondral junctions, glenoid fossae
and inferior angles of
scapulae.
|
|

|

|
Fig. 5. Lateral radiograph of dorsolumbar
spine shows increased height of the vertebral bodies with
increased density at the antero-superior and antero-inferior
margins.
|
Fig. 6. AP radiograph of legs taken at two years of age
shows only mild metaphyseal irregularity with sparing of
epiphyses and diaphyses.
|
1. Charrow J, Poznanski AK. The Jansen type
of metaphyseal chondrodysplasia: Confirmation of dominant
inheritance and review of radiographic manifestations in the
newborn and adult. Am J Med Genet 1984; 18: 321-327.
2. Lachman RS. Skeletal dysplasias–Metaphyseal
chondrodysplasia, Jansen type. In: Radiology of
Syndromes, Metabolic Disorders, and Skeletal Dysplasias, 4th edn.
Eds. Tyabi H, Lachman RS. Mosby, St. Louis, 1996; pp 852-853.
3. Nazara Z, Hernandez A, Corona-Rivera E,
Vaca G, Panduro A, Martinez-Basalo C, et al. Further
clinical and radiological features in metaphyseal
chondrodysplasia Jansen type. Radiology 1981; 140: 697-700.
4. Gordon SL, Varano LA, Alandete A, Maisels
MJ. Jansen’s metaphyseal dysostosis. Pediatrics 1976; 58:
556-560.
5. Parfitt AM, Schipani E, Rao DS, Kupin W,
Han ZH, Juppner H. Hypercalcemia due to constitutive activity of
parathyroid hormone (PTH)/PTH-related peptide receptor: Compari-son
with primary hyperparathyroidism. J Clin Endocrinol Metabl 1996;
81: 3584-3588.
6. Silverthorn KG, Houston CS, Duncan BP.
Murk Jansen’s metaphyseal chondrodysplasia with long-term
followup. Pediatr Radiol 1987; 17: 119-123.
7. Indian Council of Medical Research. Growth
and Physical Development of Indian Infants and Children.
Technical Report Series No. 18, New Delhi, Indian Council of
Medical Research, 1972,
p 67.
8. Holthusen W, Holt JF, Stoeckenius M. The
skull in Jansen type metaphyseal chondrodysplasia. Pediatr
Radiol 1975; 3: 137-144.
9. Schipani E, Jensen GS, Pincus J, Nissenson
RA, Gardella TJ, Juppner H. Constitutive activation of the
cyclic adenosine 3’, 5’–monophosphate signaling pathway by
parathyroid hormone (PTH)/ PTH-related peptide receptors mutated
at the two loci for Jansen’s metaphyseal chondrodysplasia. Mol
Endocrinol 1997; 11: 851-858.
10. Gardella TJ, Luck MD, Jensen GS, Schipani E, Potts JT,
Juppner H. Inverse agonism of amino-terminally truncated
parathyroid hormone (PTH) and PTH-related peptide (PTHrP)
analogs revealed with constitutively active mutant PTH/PTHrP
receptors. Endocrinology 1996; 137: 3936-3941.
|
