|
|
|
Indian Pediatr 2015;52: 342-343 |
 |
Late Decompensation after a Prolonged Lucid
Interval in Chronic Posterior
Fossa Extradural Hematoma
|
|
Prasad Krishnan
Department of Neurosurgery, National Neurosciences
Centre, Peerless Hospital Complex,
Kolkata, West Bengal, India.
|
|
A 6-year-old boy presented in an unconscious state with history of
holocranial headache and vomiting of two days duration. There was no
history of seizures or fever. He was afebrile but tachypneic, was
localizing with both upper limbs, with no eye opening or verbal response
(Glasgow Coma Scale of E1M5V1). Pupils were equal in size and reacting
to light. Both plantars had withdrawal response. There was a history of
fall, 3 weeks ago, following which he lost consciousness for 20 minutes
and was then apparently normal except for complaints of occipital pain
and was treated conservatively. Computed tomography (CT) scan revealed a
left-sided hypodense extra-axial mass in the posterior fossa compressing
the left cerebellar hemisphere and brain stem effacing the
perimesencephalic cistern with 4
th
ventricular shift (Fig 1). His hematological parameters
were normal. He underwent left cerebellar burr hole and evacuation of
the hematoma under general anesthesia. Intraoperatively, altered liquid
blood under pressure was drained and underlying dura was normal. A
diagnosis of chronic extradural hematoma (EDH) was made. He regained
consciousness the following day and was neurologically normal at
follow-up, two months later.
 |
| (a) |
(b) |
|
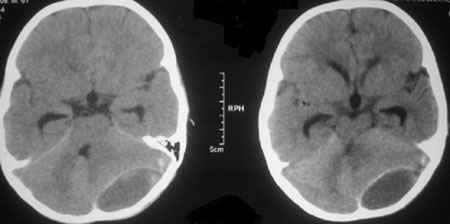
Fig. 1 Axial CT scan images (a,b)
showing a hypodense biconvex extra-axial collection in the
posterior fossa on the left side with 4 th
ventricular shift, cisternal effacement and rounding of the
third ventricle.
|
One of the well-described classical presentations of
patients with acute extra dural hematoma is a history of transient loss
of consciousness following injury with subsequent recovery for a
variable period before lapsing back into unconsciousness. This period of
transient neurological recovery is called the lucid interval and occurs
in 14-21% of patients with extra dural hematoma [1]. While there is no
consensus on how long this period may span, it has been described by
Ganz as lasting from a few hours to a few days [2]. The length of the
lucid interval will be longer if the accumulation of blood is slow, as
in venous origin of bleed or if there is significant shunting of blood
outwards through the epidural veins [2].
Given the absence of fresh bleeding (in imaging) in
this case the probable pathophysiology is expansion of the initial EDH
by fluid, flowing in down an osmotic gradient, like in a chronic
subdural hematoma leading to brain stem compression and 4th
ventricular shift.
Posterior fossa constitute around 4-13% of all
extradural hematomas [3], and sudden worsening after an initial
hypo-symptomatic period has been reported [4]. This worsening has been
reported only in the acute stage, though 11% of all extradural hematoma
become chronic over time [1]. To predict patients likely to require
surgery, Bozbuga, et al., [5] noted that acute posterior fossa
EDHs having perimesencephalic cisternal effacement and 4 th
ventricular shift were more likely to require intervention. This patient
too demonstrated both these features on imaging, though the hematoma had
become chronic.
This case was unusual because there was delayed
decompensation in the chronic stage after a prolonged lucid interval,
and that the expansion and mass effect was not related to progressive
bleed. The importance of continued close observation and follow-up
(particularly in children who cannot describe subjective symptoms
accurately) in conservatively treated extra dural hematoma is emphasized
as the symptom progression may be ‘silent and slow’ [4,5], with sudden
deterioration.
References
1. Shahlaie K, Zwienenberg-Lee M, Muizelaar JP.
Clinical Pathophysiology of Traumatic Brain Injury. In: Winn HR,
editor. Youmans Neurological Surgery. 6th ed. Philadelphia:
Elsevier, Saunders; 2011. p. 3367.
2. Ganz JC. The lucid interval associated with
epidural bleeding: evolving understanding. J Neurosurg. 2013;118:739-45.
3. Malik NK, Makhdoomi R, Indira B, Shankar S, Sastry
K. Posterior fossa extradural hematoma: our experience and review of the
literature. Surg Neurol. 2007;68:155-8.
4. Su T, Lee T, Lee T, Cheng C, Lu C. Acute Clinical
Deterioration of posterior fossa epidural hematoma: Clinical features,
risk factors and outcome. Chang Gung Med J. 2012;35:271-80.
5. Bozbuga M, Izgi N, Polat G, Gurel I. Posterior
fossa epidural hematomas: observations on a series of 73 cases.
Neurosurg Rev. 1999;22:34-40.
|
|
|
 |
|

