|
|
|
Indian Pediatr 2014;51:
312-314 |
 |
Tuberous Sclerosis Presenting with Hemorrhagic
Stroke
|
|
Radheshyam Purkait, Sreyasi Bhattacharya,
Birendranath Roy and *Ramchandra Bhadra
From Departments of Pediatric Medicine and
*Radiology, NRS Medical College and Hospital, Kolkata-700014. WB, India.
Correspondence to: Dr Radheshyam Purkait,
Email:
[email protected]
Received: December 19, 2013;
Initial review: February 04, 2014;
Accepted: March 06, 2014.
|
|
Background: Incidence of intracerebral hemorrhage in patients with
tuberous sclerosis is rare, and in most of the cases it is associated
with either underlying cerebrovascular malformation or hemorrhage into
the subependymal giant cell astrocytoma. Case characteristics: A
2-year-old boy presented with a hemorrhagic stroke, and subsequently
diagnosed as a case of tuberous sclerosis. Observation: Detailed
work-up for stroke did not reveal any definite etiology. Outcome:
Weakness gradually improved. Follow-up neuroimaging showed resolution of
hemorrhage. Message: Clinician must be aware regarding this rare
presentation of tuberous sclerosis.
Keywords: Cerebral hemorrhage, Child, Stroke.
|
|
Tuberous sclerosis complex (TSC) is an autosomal
dominant neurocutaneous syndrome with variable penetrance; the estimated
frequency is approximately one in 6,000 newborns [1,2]. Although a wide
variety of central nervous system abnormalities are associated with TSC,
intracerebral hemorrhage is rare [3-9].
Case Report
A 2-year-old boy presented with history of sudden
onset repeated vomiting, loss of consciousness, recurrent attacks of
generalized tonic-clonic seizures, and left-sided hemiparesis. There was
no history of trauma or antecedent surgery, congenital cyanotic heart
disease, dehydration, tuberculosis or bleeding disorders. Child was
previously admitted to a local hospital where he was treated with
phenytoin and aspirin. Past history revealed that he was suffering from
recurrent focal seizures since six months of age for which he was
prescribed sodium valproate, but the drug compliance was poor for the
last three months. He was born out of a non-consanguineous marriage and
had two siblings. His elder brother was also suffering from similar kind
of focal seizures since early infancy, and had profound mental
disability.
At presentation, he was afebrile but comatose with
Glasgow Coma Scale of E2V2M3 with stable vital signs, including blood
pressure. On examination, he had spasticity and weakness in the left
upper and lower limb, positive Babinski sign and exaggerated deep tendon
reflexes on the left side. Ophthalmological examination showed
mid-dilated pupils with sluggish reaction to light and bilateral
papilledema. Child had no signs of meningeal irritation or any cranial
nerve involvement. Multiple hypopigmented macules were noted over the
face, abdomen and trunk of the child. Other systemic examination was
unremarkable.
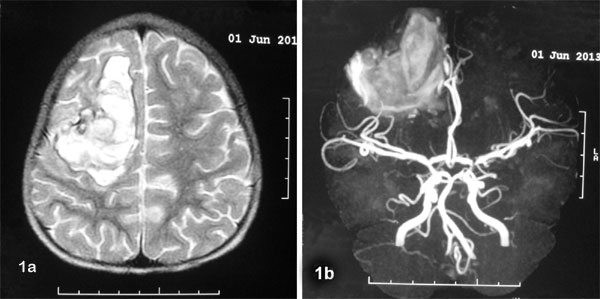
Routine hematological and biochemical investi-gations
were normal. A non-enhanced computed tomography (CT) scan of brain
showed massive acute intracranial hemorrhage with perilesional edema
located in the right fronto-parietal region with multiple
periventricular subependymal calcified nodules (Fig. 1a).
MR angiography did not detect any vascular abnormality except
intracerebral hemorrhage (Fig. 1b).
 |
|
Fig. 1 (a) Non-enhanced CT scan
showing large intracranial hemorrhage with perilesional edema
located in the right fronto-parietal region as well as multiple
periventricular subependymal calcified nodules; (b) MR
angiography showing intracranial hemorrhage in the right fronto-parietal
region without any abnormality in the major cerebral vessels.
|
Protein C and protein S level, blood lactate levels,
Carotid doppler study, and abdominal ultrasound were non-contributory.
Ophthalmological examination did not reveal any retinal abnormality. 2D
Echocardiography showed two masses, one in left ventricle of size 16×14
mm, attached to the intraventricular septum, and another (10×10 mm) in
the right ventricle suggestive of rhabdomyoma. In view of history,
clinical examination and investigations, including neuroimaging, the
child was diagnosed as a case of tuberous sclerosis. Other family
members were assessed; except mother, all had TSC but the clinical
presentations were varied. Child improved gradually on medical
management and discharged with the advice to continue sodium valproate
and physiotherapy. CT scan repeated at 3 month of follow-up visit showed
resolution of hemorrhage.
Discussion
Tuber is the characteristic brain lesion of TSC, and
may rarely differentiate into a malignant subependymal giant cell
astrocytoma. The most common neurologic manifestations are seizures,
cognitive impairment, and behavioral abnormalities, including autism
[1].
In TSC, intracerebral hemorrhage – with or without
intraventricular component – is rare. In most of the reported cases, it
was associated with either underlying cerebrovascular malformation, like
ectasia, aneurysm and arteriovenous malformation or hemorrhage into the
subependymal giant cell astrocytoma [3-9]. The underlying
pathophysiologic mechanism of intratumoral hemorrhage remains unclear;
increased venous pressure secondary to an increased intracranial
pressure is the most accepted pathogenesis leading to necrosis and
hemorrhage [6].
In the present case, neither vascular anomaly nor
intratumor hemorrhage was detected. Other possible etiologies like
hypertension, primary or metastatic central nervous system malignancy,
leukemia, coagulopathy, use of drugs like warfarin, amphetamines,
cocaine, phenypropanolamine, history of head trauma or antecedent
intracranial surgery were excluded. Although the etiology remains
unexplained in the index case, possibility of early hemorrhagic
transformation of an underlying embolic ischemic infarction could not be
ruled out as the probable pathophysiologic mechanism where cardiac
tumours were the potential source of emboli [10].
Contributors: RP: diagnosed, worked up the case
and wrote the manuscript; SB and BR: managed the case and reviewed the
literature; RP and RB: prepared the final manuscript and followed up the
case.
Funding: None; Competing interests: None
stated.
References
1. Sahin M. Tuberous Sclerosis. In: Kliegman
RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE, editors. Nelson
Textbook of Pediatrics. 19th ed. Philadelphia: Saunders; 2012.
p.2049-51.
2. Irvine AD, Mellerio JE. Genetics and
Genodermatoses: Tuberous sclerosis complex. In: Burns T,
Breathnach, Cox N, Griffiths C, editors. Rook’s Textbook of Dermatology.
8th ed. UK: Willey-Blackwell; 2010. p.15.21-25.
3. Spangler WJ, Cosgrove GR, Moumdjian RA, Montes JL.
Cerebral arterial ectasia and tuberous sclerosis: case report.
Neurosurgery. 1997;40:191-3.
4. Sabat SB, Cure J, Sullivan J, Gujrathi R. Tuberous
sclerosis with multiple intracranial aneurysms: atypical tuberous
sclerosis diagnosed in adult due to third nerve palsy. Acta Neurol Belg.
2010;110:89-92.
5. Guridi J, Tuñón M, Caballero C, Gallo-Ruiz A,
Vázquez A, Zazpe I. Intracranial hemorrhage from an arteriovenous
malformation (AVM) in a tuberous sclerosis patient. Neurologia.
2001;16:281-4.
6. Waga S, Yamamoto Y, Kojima T, Sakakura M. Massive
hemorrhage in tumor of tuberous sclerosis. Surg Neurol. 1977;8:99-101.
7. Barbosa-Coutinho LM, Lima EL, Gadret RO, Ferreira
NP. Massive intratumor hemorrhage in tuberous sclerosis. Autopsy study
of a case. Arq Neuropsiquiatr. 1991;49:465-70.
8. Kalina P, Drehobl KE, Greenberg RW, Black KS,
Hyman RA. Hemorrhagic subependymal giant cell astrocytoma. Pediatr
Radiol. 1995;25:66-7.
9. Wadhwa R, Khan IS, Thomas JO, Nanda A, Guthikonda
B. Hemorrhagic subependymal giant cell astrocytoma in a patient with
tuberous sclerosis: case report and review of the literature. Neurol
India. 2011;59:933-5.
10. Hoque R, Gonzalez-Toledo E, Minagar A, Kelley RE.
Circuitous embolic hemorrhagic stroke: carotid pseudoaneurysm to fetal
posterior cerebral artery conduit: a case report. J Med Case Rep.
2008;2:61.
|
|
|
 |
|

