|
|
|
Indian Pediatr 2014;51:
309-310 |
 |
Percutaneous Central Line Extravasation
Masquerading as an Abscess
|
|
Binu Govind, Prakash Ignace Tete and Niranjan Thomas
From Department of Neonatology, Christian Medical
College, Vellore , Tamil Nadu, India.
Correspondence to: Dr Niranjan Thomas, Professor,
Department of Neonatology, Christian Medical College Hospital, Vellore
632 004, Tamilnadu, India.
Email:
niranjan@cmcvellore.ac.in
Received: December 19, 2013;
Initial review: January 07, 2014;
Accepted: February 05, 2014.
|
|
Background: Percutaneous central line insertion is a common
procedure in the neonatal intensive care unit. Case characteristics:
A preterm baby, who had a percutaneous central line inserted developed
an erythematous swelling over the infraclavicular area. Observation:
A diagnosis of abscess was made, and an incision and drainage done that
revealed a white fluid with high triglyceride content, confirming lipid
extravasation. Outcome: The lesion healed completely few days
after removal of the catheter. Message: This case highlights the
importance of proper placement and confirmation of central line
position.
Keywords: Central venous line, Complication,
Abscess, Total parenteral nutrition.
|
|
Percutaneously inserted central catheters (PICC)
are commonly used in the neonatal intensive care units (NICU) to
administer hyperosmolar solutions, total parenteral nutrition (TPN) and
medications. However, PICCs have been associated with complications due
to displacement, embolism, thrombosis or infection of the catheter [1].
Effusions into a body cavity can occur when a PICC passes into a small
vein and damage the vascular wall occurs. Extravasation into pleural,
pericardial, subdural and retroperitoneal, and renal pelvis have been
described. [2-4] Central line migration and extravasation leading to
superficial abscess is extremely rare [5]. We report a child who
presentedwith a chest wall swelling which was due to extravasation of a
malpositioned PICC into a superficial vein of the chest wall.
Case Report
The patient was the first of twins, born to a
primigravida mother who had regular antenatal care in our hospital. The
mother had spontaneous onset of labour at 29weeks of gestation and baby
was born by assisted breech delivery with a birthweight of 1280g and
APGAR scores of 2, 6 and 7 at 1, 5 and 10 minutes, respectively. He was
admitted into the NICU for preterm care and respiratory distress. He
received 70 hours of continuous positive airway pressure for moderate
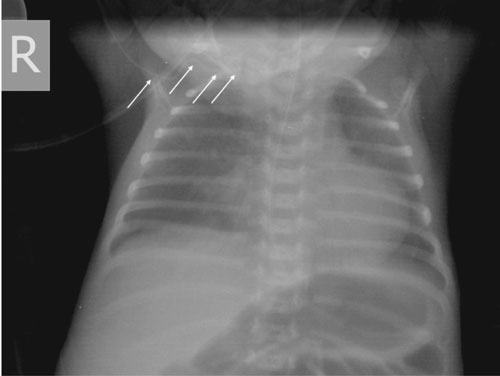
hyaline membrane disease, and antibiotics for presumed sepsis. A right
brachial PICC (Vygon, 2 Fr) was inserted and position was confirmed
radiologically to be in the subclavian vein (Fig. 1) and
TPN infusion was started. On day 27 of life, baby was noted to have an
erythematous swelling in the right infraclavicular region. Pediatric
surgery consultation was obtained, and incision and drainage was done in
view of a clinical diagnosis of abscess. A whitish coloured fluid was
seen draining out and on flushing the PICC line, a fluid similar in
appearance to lipid infusate was noted to be coming out (Fig.
2). Triglyceride estimation of the sample aspirated from the site
was high (756 mg/dL), confirming that the fluid was extravasating TPN.
The PICC line was removed and the drainage site started healing
gradually. He was discharged on day 66 of life on breast feeds when he
was gaining weight adequately. At follow-up of 18 months, the child is
neurodevelop-mentally normal.
 |
 |
|
Fig. 1 X-ray of the chest and abdomen
showing the position of the PICC appearing to be in the right
subclavian.
|
Fig. 2 Infraclavicular swelling with
extravasating intralipid after the incision and drainage.
|
Discussion
PICC is useful in the care and nutrition of sick and
small neonates, and is one of the common procedures done in the NICU.
The ideal position for catheters inserted through the upper limb is at
the junction of superior vena cava (SVC) and right atrium while those
inserted through the lower limb line should be in the inferior vena cava
(IVC) at the level of diaphragm [3,6]. Risks involved in the use of PICC
lines include infection, thrombosis, vessel perforation and
extravasations [1]. Factors implicated in causing the vessel perforation
and subsequent extravasation include occlusive mural thrombosis,
localized phlebitis and erosion of the vessel wall by the catheter. When
the end of the catheter creates an acute angle with the vessel wall, the
jet of abrasive fluid directed on the wall may lead to formation of a
thrombus attaching the catheter tip to the vessel endothelium [1]. This
is more likely to occur if the catheter is in a smaller vessel with a
slower flow of blood.
There have been reports of PICC extravasation causing
pericardial effusion and also leakage of fluid into subdural space,
renal pelvis, peritoneal cavity, retroperitoneal space and pleural space
[3,4]. Extravasations into soft tissue have been reported less
frequently. Baker, et al.[5] have described extravasation of a
lower limb PICC presenting as an abdominal wall abscess similar to the
presentation seen in our patient.
In our case, the initial position of the PICC was
thought to be in the subclavian vein but was probably malpositioned into
a superficial vein of the chest. This highlights the fact that optimal
position of the PICC should always be ensured. Blind positioning of PICC
based on anatomical landmarks and anthropometry leads to high
malposition rates [7]. Single plane X ray alone may not be adequate in
identifying the central line. In one series, 50% of line tips were not
identified by plain X-ray; radio-opaque contrast injection
increased detection rates to 93.5% [8]. Odd, et al.[9] showed
radio-opaque contrast to increase the proportion of central line tip
position identification from 39% to 55%. Groves, et al.[10] have
described easy localization of the PICC line tip using colour doppler
ultrasound with the line being flushed with saline at a rate of 0.1 mL/s.
To avoid complications, either contrast injection or bedside ultrasound
with colour doppler may be used to identify the central line tip
position. Confirmation of central line tip and daily inspection by
experienced personnel will help prevent delay in identification of
complications [1].
Contributors: All the authors were
involved in the diagnosis and management of the patient.
Funding: None; Competing interests: None
stated.
References
1. Menon G. Neonatal long lines. Arch Dis Child Fetal
Neonatal Ed. 2003;88:F260-2
2. Madhavi P, Jameson R, Robinson MJ. Unilateral
pleural effusion complicating central venous catheterization. Arch Dis
Child Fetal Neonatal Ed. 2000;82:F248-9.
3. Nowlen TT, Rosenthal GL, Johnson GL, Tom DJ, Vargo
TA. Pericardial effusion and cardiac tamponade in infants with central
catheters. Pediatrics. 2002;110:137-42.
4. Nadroo AM, al-Sowailem AM. Extravasation of
parenteral alimentation fluid into the renal pelvis-a complication of
central venous catheter in a neonate. J Perinatol. 2001;21:465-6.
5. Baker J, Imong S. A rare complication of neonatal
central venous access. Arch Dis Child Fetal Neonatal Ed. 2002;86:F61-2.
6. Ramasethu J. Complications of vascular catheters
in the neonatal intensive care unit. Clin Perinatol. 2008;35:199-222.
7. Johnston AJ, Bishop SM, Martin L, See TC, Streater
CT. Defining peripherally inserted central catheter tip position and an
evaluation of insertions in one unit. Anaesthesia. 2013;68:484-91.
8. Reece A, Ubhi T, Craig AR, Newell SJ. Positioning
long lines: contrast versus plain radiography. Arch Dis Child Fetal
Neonatal Ed. 2001;84:F129-130.
9. Odd DE, Page B, Battin MR, Harding JE. Does
radio-opaque contrast improve radiographic localization of percutaneous
central venous lines? Arch Dis Child Fetal Neonatal Ed. 2004;89:F41-43.
10. Groves AM, Kuschel CA, Battin MR. Neonatal long
lines: localisation with colour Doppler ultrasonography Arch. Dis Child
Fetal Neonatal Ed. 2005;90:F5.
|
|
|
 |
|

