Germinomas are the commonest primary intracranial
germ cell tumors and account for over 50% of all neoplasms in the region
of pineal gland. The preferential locations of intracranial germinomas
are the pineal and suprasellar regions.
Germ cell tumors with synchronous lesions in the
pineal and suprasellar regions (GCTSPS) account for nearly 10% of all
intracranial germ-cell tumors(1,2). There is a male predominance with
majority of the patients presenting in the second decade of life. We are
presenting a rare case of synchronous germinoma in the pineal and
suprasellar region in an 11-year-old male child.
Case Report
A 11-year-old boy presented with polyuria and
polydipsia of three months duration, and headache, nausea, vomiting,
blurred vision and unsteady gait of one month duration. Neurological
examination revealed papilledema and bilateral scotoma. There was
restriction of upward gaze and convergent nystagmus on attempted upgaze
(Parinaud’s syndrome). The patient had normal mental development and
secondary sexual characters.
The routine hematological examination revealed no
abnormality. The CSF examination did not show any abnormal cells. The
serum alpha-protein level was raised (1.1 ng/mL). b-hCG level was also
significantly elevated to 988 MIU/mL.
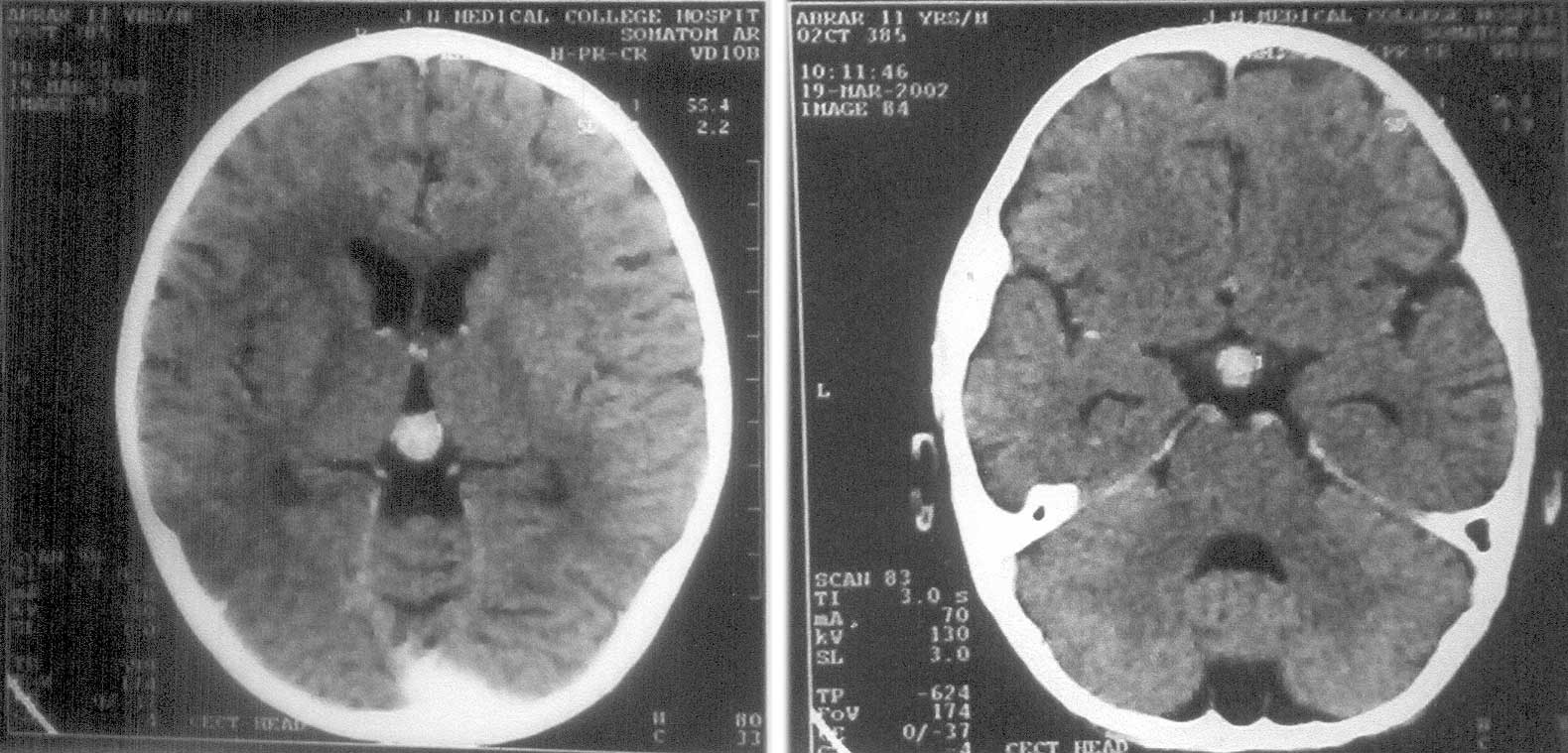
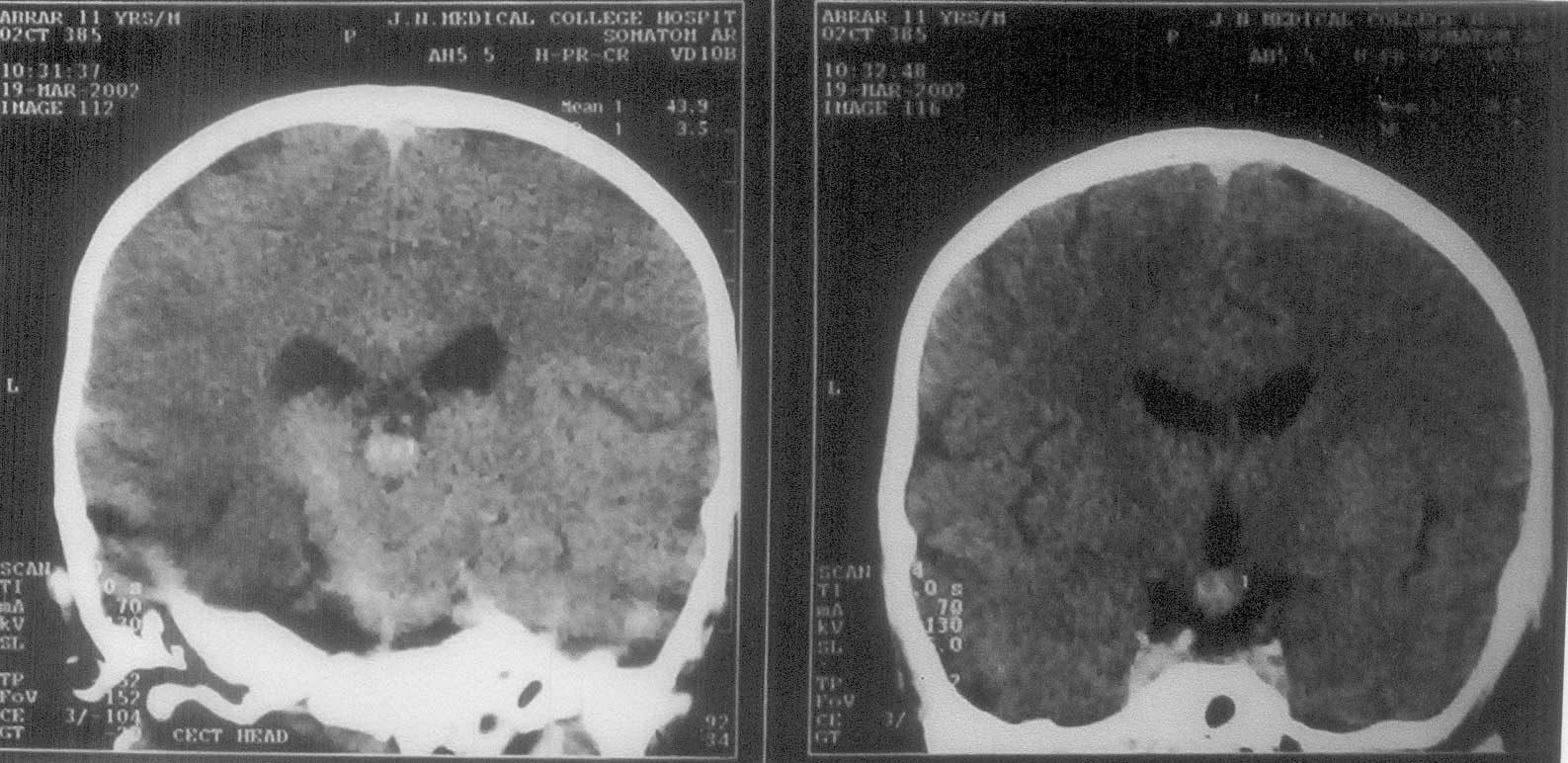
CECT head (Fig. 1) showed well defined rounded
homogenously enhancing lesion, in the pineal and suprasellar region
measuring l.3 × 1.0 cm and 1.0 × 1.1 cm respectively, without any
evidence of calcification or necrosis. The suprasellar lesion was
causing mass effect on the floor of 3rd ventricle. Bilateral temporal
horns were mildly prominent. Craniotomy was performed and tumor was
resected through subfrontal approach, which on histopathology revealed
germinoma and subsequently the patient was put on radiotherapy.
 |
 |
|
Fig.1(a,b). Axial and coronal post contrast
CT scans demonstrating well defined markedly enhancing suprasellar
and pineal masses, with mass effect on third ventricle. |
Histopathologic examination of multiple, irregular,
grayish brown soft tissue bits revealed the tumor to be composed of two
types of cells–polyhedral cells with vacuolated cytoplasm and cells
identical to small mature T-lymphocytes. They were arranged in lobules
traversed by delicate vascularized trabeculae.
Discussion
The term "germinoma" was originally introduced by
Friedman(3). Majority of the patients presents in the second decade of
life, with a preponderance of males over females(1). The symptoms depend
on the location of the tumor within the brain. In the suprasellar
germinoma, endocrinological manifestations prevail (most commonly
diabetes insipidus, delayed gonadal functions and precocious puberty may
be the other complaints). Symptoms in germinomas located in the pineal
region are due to increased intracranial pressure(4). When the tumor
involves both sellar and the pineal region, the presenting symptoms are
typically due to sellar lesion rather than the pineal mass. The present
case an 11 years old boy also initially presented with features due to
sellar mass particularly diabetes insipidus and subsequently developed
features due to raised ICT. Involvement of the oculomotor apparatus
produces loss of upward conjugates deviation of the eyes (Parinaud’s
syndrome) and abnormal pupillary reflexes(5). Our patient had most of
the common clinical features described by Sung, et al.
Intracranial germinomas may also be associated with Down’s syndrome(6).
The introduction of CT scanning was truly an epoch,
though MRI is the ideal investigation today. On plain CT, the tumor
shows well defined, rounded and homogenous is to slightly higher density
mass. Calcification and necrosis are rare. After intravenous contrast
administration, the tumor shows homogenous enhancement irregular margins
suggest local infiltration. MR scans typically demonstrate an
infiltrating mass that is isointense to brain on T1WI, moderately
hyperintense on T2WI and enhances strongly and homogenously after
contrast adminis-tration(7). GCTSPS has been considered highly sensitive
to irradiation and can be cured with it alone without histological
diagnosis. However, some subtypes are not radiation sensitive and
neuroimaging characteristics of germinoma and non germinomatous tumors
are similar enough to limit diagnostic certainty and proceeding for
further treatment on its basis alone. So, histopathological
confirma-tion becomes significant atleast from single site. Keeping this
in view, we also got the histopathology done from only the suprasellar
region. The histologic picture is highly distinctive. About 70% to 80%
of tumor-infiltrating lymphocytes in intracranial germinomas are
T-lymphocytes and 20 to 30% are B-lymphocytes.
In pineal region germ cell tumors cannot be separated
on the basis of neuro-imging characteristics from other tumors such as
pineablastoma, pineocytomas or gliomas. However, pattern of
calcification may be helpful in differentiating them(8). Differential
diagnosis of a suprasellar region germinoma includes opticochiasmatic -
hypothalamic glioma and cranio-pharyngiomas. Langerhans cell
histiocytosis may clinically and radiographically mimic it but isolated
disease of the central nervous system in Langerhans cell histiocytosis
is rare(8).
Ideal treatment of germinoma consists of surgical
removal, post-operative chemo-therapy and craniospinal radiotherapy.
Over-all prognosis of this tumor is good with 90% 5 year survival rate.
Non-gerrninomatous germ cell tumors have a worse prognosis, with 5yrs
survival rates less than 25%(8). Blood hCG and alpha-fetoprotein levels
are useful markers for follow-up.
Contributors: FH diagnosed the case and
supervised the manuscript and is guarantor of the paper: SAA & MZ
reviewed the literature and prepared this manuscript and followed the
patient. SN performed histopathological examination.
Funding: None.
Competing interests: None.
