Introduction
Tracheo-bronchial rupture, due to blunt trauma in
children, is an uncommon injury with a variety of clinical
presentations(1-3). The clinical features even with the major
disruptions can be minimal, delaying the diagnosis in 25 to 68% of the
cases and hence, high index of suspicion is required for diagnosis(1,4).
However, a total absence of initial clinical signs and symptoms is
unusual. We present a case of right main bronchus injury with absence of
initial clinical features resulting in a delayed diagnosis.
Case Report
An 8-year-old, 13 kg boy sustained blunt trauma with
an iron door falling on his chest and pinning him to the ground. There
was no history of head injury, respiratory distress, subcutaneous
emphysema or hemodynamic instability following trauma and the chest
radiograph did not reveal pneumothorax or pneumomediastinum. He was
given pain relief and did not require hospitalization. The child
remained well for 3 months before he started having recurrent cough and
occasional difficulty in breathing on exertion. The patient was treated
symptomatically for another 5 months in a peripheral hospital before
referral to our center. The clinical examination revealed a stable child
with no respiratory distress. The chest wall on the right side was
slightly depressed. The trachea and heart were shifted to the right and
the air entry was poor in the right lower half of the chest. An x-ray
of the chest revealed collapsed right lung near the right dome of the
diaphragm and hyper-inflation of the left lung. The underlying bony cage
was normal. An ultrasonography of the chest showed minimal fluid in
right thoracic cavity. The echocardiography was normal. The CT scan of
the chest showed collapsed right lung lying in the right para-vertebral
gutter and hyper-inflated left lung with herniation of the apex of left
lung to the opposite side. The right main bronchus showed abrupt cut-off
with no evidence of extrinsic compression or endo-bronchial lesion
including foreign body thereby suggest-ing a bronchial injury (Fig. 1).
Bronchoscopy revealed normal trachea and bronchial take-off on both the
sides but the right main bronchus was completely occluded at 1.5 cm from
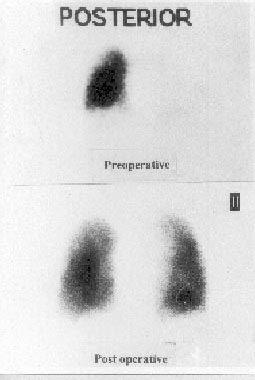
the carina. The origin of upper lobe bronchus was not seen. A perfusion
scan of the lung showed negligible perfusion (only background activity)
to the collapsed right lung (Fig. 2).
 |
|
Fig. 1. CT scan of chest showing herniation
of hyperinflated left lung and atelectatic right lung in right
paravertebral gutter. |
The endotracheal tube for general anesthesia was
manipulated into the left main bronchus. The patient underwent right
postero-lateral thoracotomy. The right main bronchus was found to be
transected at about 1.5 cm from the carina, and the other end was
somewhat buried into the collapsed lung near its hilum. The gap between
the two ends was approximately 4 cm. The distal end was dissected out
from the hilar structures and opened. After suction of the mucus, the
collapsed lung could be inflated by inserting a separate endotracheal
tube into the distal bronchial end. An end-to-end anastomosis was
performed with interrupted sutures of 5-0 Vicryl in a single layer.
Post-operatively, the patient recovered well and did not require
ventilation. A perfusion scan four months later showed near-normal
expanded lung with increased perfusion (Fig. 2). The chest
radiograph and the CT scan showed near normal lung expansion and the
patient had developed normal exercise tolerance.
 |
|
Fig. 2. Radionucleide perfusion scan showing
majority of the perfusion going to the left lung preoperatively
(upper scan) and near equal perfusion of both the lungs 4 months
after repair (lower scan). |
Discussion
The patients with traumatic rupture of tracheo-bronchial
tree exhibit well-recognized signs and symptoms of bronchial transection
such as shortness of breath, mediastinal and subcutaneous emphysema,
hemoptysis, pneumothorax, atelectasis, persistent air leak and failure
to expand the lung with thoracostomy tube drainage. The lung drops below
the level of the carina if the bronchus is completely transected and it
is a pathog-nomonic radiological sign(1,5,6). Various mechanisms of
injury are compression of tracheobronchial tree between the sternum and
the vertebral column resulting in distraction of the carina, shearing of
bronchus by rapid deceleration and rapid increase in tracheo-bronchial
pressure as a result of crush injury with a closed glottis(1,5).
The bronchial injury may be sealed by the
peribronchial tissues and the patient survives the initial damage but
absence of air leak at presentation is unusual and rare(6,7). However if
the tear is in the mediastinal part of the main bronchus or trachea,
pneumothorax may not occur and only mediastinal air will be seen(3,5).
In cases, which have no pleural communication, ventilation may proceed
through the torn area and the diagnosis is frequently delayed(5).
Bronchoscopy is mandatory to make the diagnosis of bronchial transection
when such a lesion is suspected even with minimal clinical and radio-
logical symptoms(1-3,6). Granulation tissue invades the area over next 1
to 3 weeks after injury. Incomplete obstruction will lead to restriction
of normal removal of the secretions and infection. However, if the
bronchial communication snaps suddenly and completely, there is no
aeration, which protects the lung from the air-borne sepsis and sterile
mucus collects inside the atelectatic lung(5). The possibility of
bronchial repair should be entertained even in the cases recognized long
after injury(6). The prognosis depends upon the time interval between
the diagnosis and treatment, associated vessel injury and the condition
of the distal transected lung(6). Expansion and deflation of the lung on
the operation table, before repair, demonstrates compliance and
elasticity of the atelectatic lung and the likelihood of regaining a
good lung growth in the postoperative period. When repair is
impractical, resection is indicated to avoid infection and pulmonary
vascular shunt(1).
The vascularity of the chronic atelectatic lung is a
concern especially in the cases, which are diagnosed late(8). The
radionucleide perfusion scan is a simple, efficient, non-invasive
modality to evaluate the circulation of chronically collapsed lung and
can be used repeatedly to assess the immediate and delayed response to
the surgical repair(4,5).
In our case, the initial symptoms were subtle and the
child did not show the air leak either clinically or radiologically, to
suggest the presence of tracheo-bronchial disruption. Such near total
absence of clinical symptoms has been unusual in the pediatric
population. The diagnosis is usually delayed if air ceases to leak from
the chest drainage tube, which our patient did not require. However,
persistent atelectasis of the lung in our patient aroused the suspicion
of a bronchial injury and bronchoscopy confirmed it. Hence, significant
bronchial injuries may occur in the absence of usual initial symptoms.
Therefore, the patients of obvious chest trauma should be on follow up
in the immediate post-injury period for detecting these lesions to avoid
unnecessary morbidity and possible mortality.
Contributors: Study concept and design JKM, KLNR,
PM, BRM. Analysis and interpretation of data: JKM, KLNR, PM, BRM.
Drafting of manuscript: JKM, PM, KLNR, Guarantor of the manuscript: KLNR.
Funding: None.
Competing interests: None stated.
