|
Intracerebral Hydatid Cyst in a Child with Atrial Septal Defect |
Tufail Patankar
Niketa Chotai
Srinivasa Prasad
Sheena Chowdhry
Atul Goel*
From the Departments of Radiology, and *Neurosurgery, King Edward Memorial Hospital, Parel, Mwnbai 400 0 12, India.
Reprint requests: Dr. T. Patankar, Department of Radiology, King Edward Memorial Hospital, Mumbai 400 0 I 2, India.
Manuscript Received: March 7,1998; Initial review completed: June 16, 1998;
Revision Accepted: September 18, 1998
Brain involvement in hydatid disease occurs in 1-2% of all echinococcus infections. Between 50-75% of all intracranial
hydatid cysts are seen in children(1). The occurrence of cerebral hydatid cyst in a patient with patent ductus arteriosus was first reported by Lunardi et al.(2).
We report a child with intracerebral hydatid cyst who had atrial septal defect (ASD).
Case Report
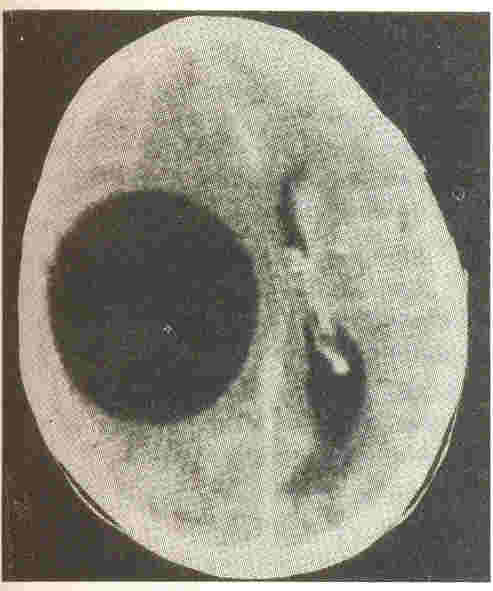
A 9-year-old boy with ASD, diagnosed on
2D echocardiography, presented with left hemiparesis of three months duration. Clinical examination revealed left sided spastic hemiparesis, UMN type of facial palsy and an extensor plantar reflex on the left side. Other Cranial nerves were normal. Fundus examination was unremarkable. CSF study was normal. A contrast enhanced CT scan of the brain showed a large, non enhancing, smooth marginated, cystic (8 HU) lesion in the right parietal cortex (Fig. 1). It caused compression of the frontal horn of the ipsilateral lateral ventricle. There was no perifocal edema. A
diagnosis of intracerebral hydatid cyst was suggested. Radiological evaluation of the chest and abdomen did not show hydatid disease. The cyst was surgically removed in toto from its bed by hydrostatic excision, taking care to avoid rupture. Histological examination
of the cyst revealed typical double layered wall with few brood capsules within it, confirming the CT diagnosis of hydatid cyst. A repeat CT scan of the brain after six months showed no evidence of recurrence.
 |
|
Fig. I. Contrast enhanced CT scan of the brain demonstrating, a large, cystic
mass lesion in the right parietal cortex. Note the absence of
perifocal edema. |
Discussion
Hydatid disease is cause by the larval form of Echinococcus granulosus/Echinococcus multilocularis. While the dog is the definitive host, sheep, cattle and occasionally humans serve as intermedite hosts. The prevalence of hydatid disease is high, especially in sheep and cattle raising countries. The ingested ova reach the small intestine, where the liberated
embryos penetrate the mucosa, and reach the portal circulation. Later systemic, hematogenous dissemination ensues.
Intracranial hydatid cysts account for 1-2% of all Echinococcus granulosus infections( 1). Lunardi etal.(2)
in their study of intracerebral hydatid cysts in 12 children found one patient with patent ductus arteriosus. They suggested that the presence of cardiac shunt predisposed to the occurrence of primary brain hydatid cyst in children. On review of literature, we did not find any other similar reports. Our patient had ASD and we believe that this might have contributed to his primary brain hydatid cyst, possibly due to paradoxical embolism, a well reported cause of stroke in young patients(3,4).
In the brain, hydatid cysts are usually con- fined to the supratentorial compartment; in the region supplied by middle cerebral artery. the parietallobe(5) is especially involved, as was the case in our patient. Hydatid cysts in the brain usually do not calcify. Occasional perifocal edema may be seen; especially in recurrence( 1). The development of symptoms and neurologic deficits is usually late and is due to raised intracerebral tension.
The correct preoperative diagnosis can be established by CT scan and obviates the need for diagnostic aspiration which is hazardous(5). The differential diagnoses in a child include abscess, cystic neoplasm and porencephalic cyst. The absence of perifocal edema and enhancement differentiates it from an abscess. Porencephalic
cysts usually communicate with the ventricular system. Tumors occassionally may be cystic but are nearly always associated with a soft tissue mass(2). CT scan not only helps in diagnosis with high accuracy,
but also identifies the most superficial part of the cyst for a cortical
incision and minimizes the risk of rupture at surgery. Specific
diagnosis is best achieved by histological examination. The treatment of hydatid cyst is exclusively surgical(2). The surgical challenge is to remove the cyst intact. Spillage of its contents can result in anaphylactic shock and the spillage of the scolex bearing fluid may result in systemic dissemination.
|
1.
Ersahin Y, Mutluer S, Guzelbag E. Intracranial hydatid cysts in children. Neurosurgery 1993; 33: 219-224.
2.
Lunardi P, Missori P, Lorenzo ND, Fortuna A.
.
Cerebral hydatidosis in children: A retrospective survey with emphasis on long term follow-up. Neurosurgery 1991; 29: 515-518.
3.
Schminke U, Daffertshofer M, Hennerici M. Distribution of cerebral ischemia in the posterior and anterior circulation in patients with paradoxical embolism. Cerebrovasc Dis 1996; 6 (SuppI2): 164.
4.
Bohnichon P, Meyniard 0, Boissonnas A. Cazil1 B, D Enfert J, Chapuis Y. Paradoxical embolism associated with an interatrial
communication. Press Med 1984; 13: 684.
5.
Sharma S, Ray RC. Primary hydatid cyst of the brain in an' adult: Report of a case. Neurosurgery 1991;
23: 374-376.
|
